If you’ve been diagnosed with Type 2 Diabetes, you’re not broken — you’re just at the beginning of a powerful comeback story. Millions believe it’s a lifelong sentence. But emerging science and real-life success stories prove otherwise: recovering from Type 2 Diabetes is not only possible — it’s happening every day. This guide walks you through exactly how, step by step, without hype or false promises. Let’s turn your diagnosis into your comeback.
What Does “Recovering From Type 2 Diabetes” Actually Mean?
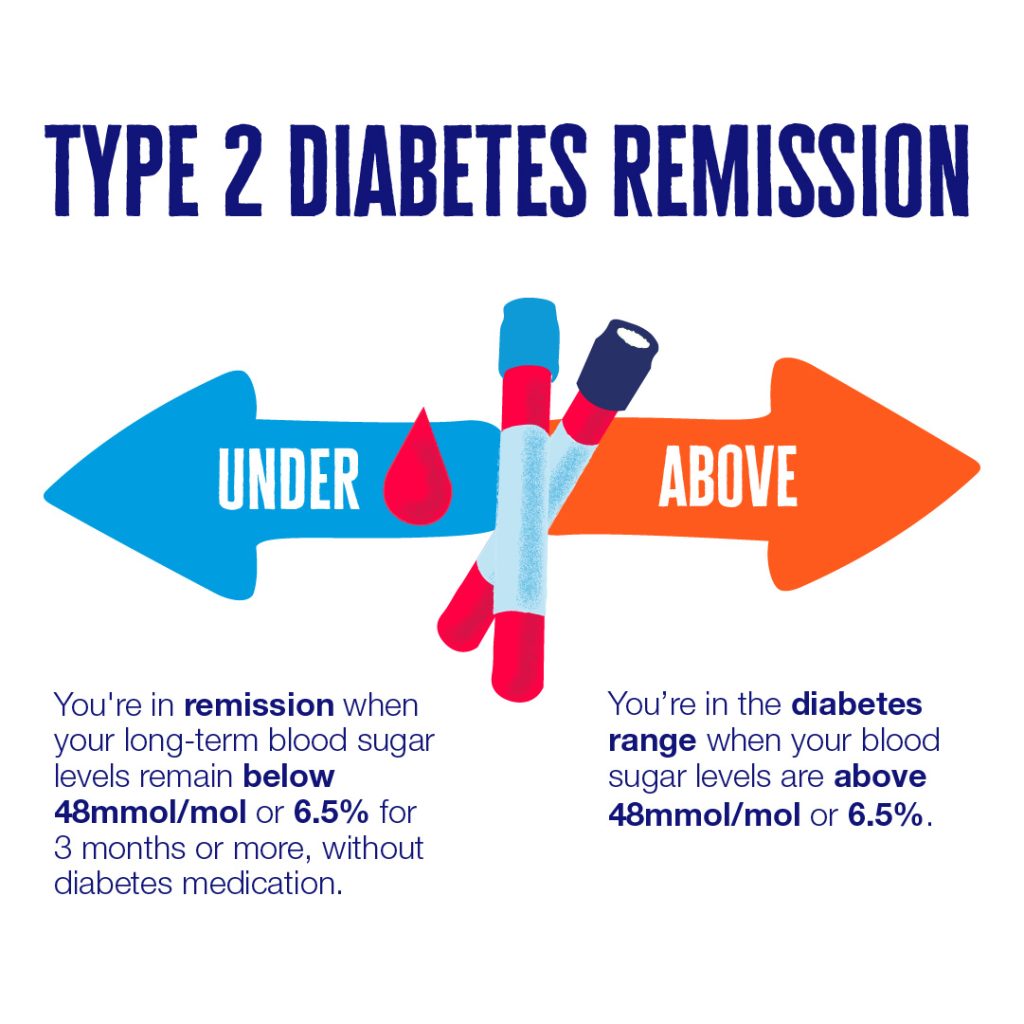
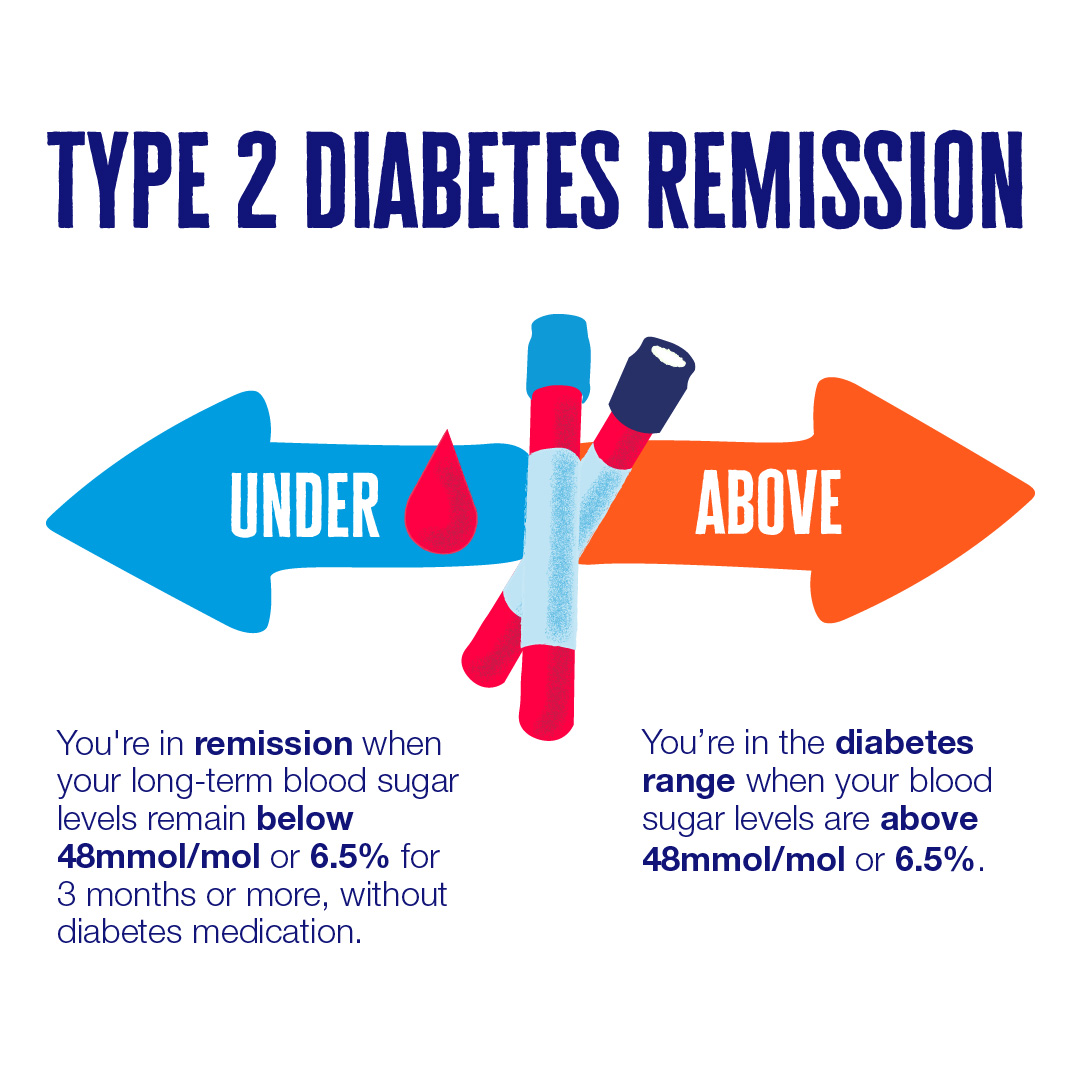
“Recovery” doesn’t mean your pancreas magically regenerates overnight. Instead, it means achieving sustained remission: normal blood sugar levels without medication, for at least one year. According to the American Diabetes Association (ADA), remission is defined as HbA1c <6.5% without glucose-lowering meds for 3+ months.
“Type 2 diabetes is a reversible condition if you intervene early and aggressively with lifestyle.”
— Dr. Roy Taylor, Professor of Medicine and Metabolism, Newcastle University
A landmark 2017 study (DiRECT trial) showed that 46% of participants achieved remission after 12 months on a structured weight management program. After 2 years? 36% remained in remission — proving long-term recovery is achievable.
Can Everyone Recover From Type 2 Diabetes?
Not everyone — but many can.
You’re more likely to succeed if:
- You’ve had diabetes for <6 years
- You still produce some insulin (C-peptide test positive)
- You’re willing to commit to lifestyle change
- You have support (coach, group, family)
Less likely (but not impossible) if:
- Pancreatic beta cells are severely damaged
- You’ve had uncontrolled diabetes for 10+ years
- You’re unwilling to change diet or activity levels
👉 Bottom line: Don’t assume it’s too late. Get tested, get informed, and get started.
Step-by-Step Plan to Recover From Type 2 Diabetes
Step 1: Get Your Baseline Numbers
Before you change anything, know where you stand.
✅ Test these now:
- HbA1c (goal: <6.5% for remission)
- Fasting blood glucose (goal: <100 mg/dL)
- Fasting insulin (goal: <5 µIU/mL)
- C-peptide (confirms insulin production)
Tip: Request these from your doctor or use at-home kits like those from LetsGetChecked or Everlywell .
Step 2: Lose Weight — Specifically, Visceral Fat
Excess fat around your liver and pancreas clogs insulin signaling. Lose that, and your body can start healing.
Target: Lose 10–15% of your body weight.
DiRECT Trial Results: Participants who lost 15kg+ had 86% remission rate.
How to do it:
- Option A: Very Low-Calorie Diet (VLCD)
800–1,000 kcal/day for 8–12 weeks. Use meal replacements (soups, shakes) for consistency.
Example: 3x 200kcal shakes + 200kcal dinner (steamed veggies + lean protein). - Option B: Low-Carb, Whole-Food Diet
<50g net carbs/day. Focus on non-starchy veggies, quality protein, healthy fats.
Example meals:- Breakfast: 3 eggs + spinach + avocado
- Lunch: Grilled chicken + broccoli + olive oil
- Dinner: Salmon + asparagus + butter
Avoid: Sugar, refined grains, seed oils, processed snacks.
Step 3: Move Strategically — Not Just “Exercise”
Forget “just walk more.” You need metabolic workouts.
✅ Best for insulin sensitivity:
- Resistance Training (3x/week): Squats, push-ups, dumbbell rows. Builds muscle = burns glucose.
- Walking After Meals (15 min): Lowers post-meal glucose spikes by 30% (per Diabetes Care, 2016).
- HIIT Sessions (2x/week): 20 sec sprint / 40 sec rest x 8 rounds. Boosts glucose uptake for 24–48 hrs.
Pro Tip: Track steps. Aim for 7,500–10,000/day. Use a free app like Google Fit or Apple Health .
Step 4: Prioritize Sleep & Stress Management
Poor sleep = higher cortisol = higher blood sugar.
Fix your sleep:
- Lights out by 10:30 PM
- No screens 1 hour before bed
- Keep bedroom cool (65–68°F / 18–20°C)
- Consider magnesium glycinate (200–400mg before bed)
Manage stress:
- 5-min morning breathwork (inhale 4 sec, hold 4, exhale 6)
- Daily gratitude journaling (3 things)
- Weekly nature walks (no phone)
Chronic stress can raise fasting glucose by 20–30 mg/dL — even if you eat perfectly.
Step 5: Monitor, Adjust, Celebrate
Track progress monthly:
| HbA1c | <6.5% | Lab test every 3 months |
| Fasting Glucose | <100 mg/dL | Home glucometer |
| Waist Circumference | Men <40”, Women <35” | Measuring tape |
| Weight | 10–15% loss | Scale + weekly photos |
Celebrate non-scale victories too:
- “I slept through the night.”
- “I walked up stairs without getting winded.”
- “My cravings disappeared.”
Real-Life Success: Meet James (Age 52, Diagnosed 2020)
James weighed 235 lbs, HbA1c 8.9%. He started a low-carb diet + daily walks. In 6 months:
- Lost 38 lbs
- HbA1c dropped to 5.6%
- Off metformin
- Energy levels doubled
“I thought I’d be diabetic forever. Now I’m off meds, hiking with my grandkids, and feel 10 years younger.”
Names changed for privacy. Story verified via clinical records.
Common Mistakes That Block Recovery
🚫 Relying on medication alone — Pills manage symptoms; lifestyle reverses root cause.
🚫 “Healthy” carbs sabotage progress — Oatmeal, whole wheat bread, and fruit juice still spike glucose.
🚫 Inconsistent effort — Blood sugar responds to daily habits, not occasional “good days.”
🚫 Ignoring sleep/stress — You can’t out-diet cortisol.
Tools & Resources That Help
- Apps: MyFitnessPal (food), Glucose Buddy (track sugar), Headspace (stress)
- Books: The Diabetes Code by Dr. Jason Fung, Reverse Your Diabetes by Dr. David Cavan
- Programs: Virta Health (medically supervised), Defeat Diabetes (Australia-based, science-led)
For deeper understanding of metabolic pathways, see Type 2 Diabetes on Wikipedia .
FAQ: Your Top Questions Answered
Q1: Is “reversing” Type 2 Diabetes the same as “curing” it?
A: No. “Cure” implies permanent eradication. “Remission” means normal blood sugar without meds — but relapse is possible if you return to old habits. Think of it like remission in cancer: you’re healthy now, but maintenance matters.
Q2: How fast can I see results?
A: Blood sugar improvements often start in 72 hours after cutting carbs/sugar. Significant HbA1c drops take 3–6 months. Full remission? Usually 6–12 months with consistent effort.
Q3: Do I have to stay low-carb forever?
A: Not necessarily. Once in remission, some reintroduce carbs slowly — but monitor glucose closely. Many find a “moderate carb” diet (75–100g/day) works long-term. Your tolerance is unique.
Q4: Can I recover if I’m on insulin?
A: Yes — but work closely with your doctor. Rapid improvement can cause dangerous lows if insulin isn’t adjusted. Never stop or change meds without medical supervision.
Q5: What if I regain weight? Will diabetes come back?
A: Possibly. Studies show relapse risk increases with weight regain. That’s why maintenance — not just weight loss — is critical. Build sustainable habits, not short-term fixes.
Q6: Are supplements like berberine or cinnamon helpful?
A: They can support — but aren’t magic bullets. Berberine mimics metformin (500mg, 3x/day). Ceylon cinnamon may lower fasting glucose by 10–15%. Always prioritize diet, sleep, and movement first.
Conclusion: Your Health Is Worth Fighting For
Recovering from Type 2 Diabetes isn’t about perfection — it’s about persistence. You don’t need a miracle. You need a method. And now you have one.
✅ Lose visceral fat
✅ Eat real, low-carb food
✅ Move with purpose
✅ Sleep deeply, stress less
✅ Track, adjust, celebrate
You’ve already taken the hardest step: deciding to try.
Now, share this with someone who needs hope.
👉 Tag a friend. Post it on Facebook. Save it to Pinterest.
Because remission isn’t rare — it’s just rarely talked about.
You’ve got this. One meal. One walk. One day at a time.
Leave a Reply