Finding out you have gestational diabetes mellitus (GDM) during pregnancy can feel overwhelming—even scary. You’re not alone. In fact, up to 10% of pregnancies in the U.S. are affected by GDM, according to the CDC. This article shares a real, personal experience of a patient diagnosed with gestational diabetes mellitus—what it felt like, how she coped, and what actually worked. If you’ve just received a diagnosis or know someone who has, this story offers empathy, practical steps, and hope.
What Is Gestational Diabetes Mellitus—and Why Did It Happen to Me?
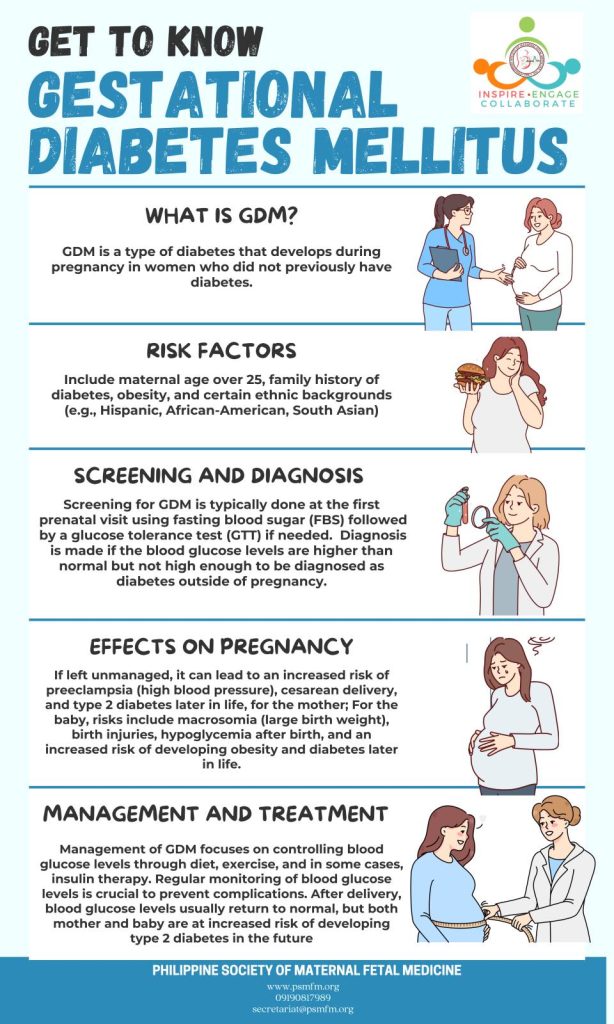
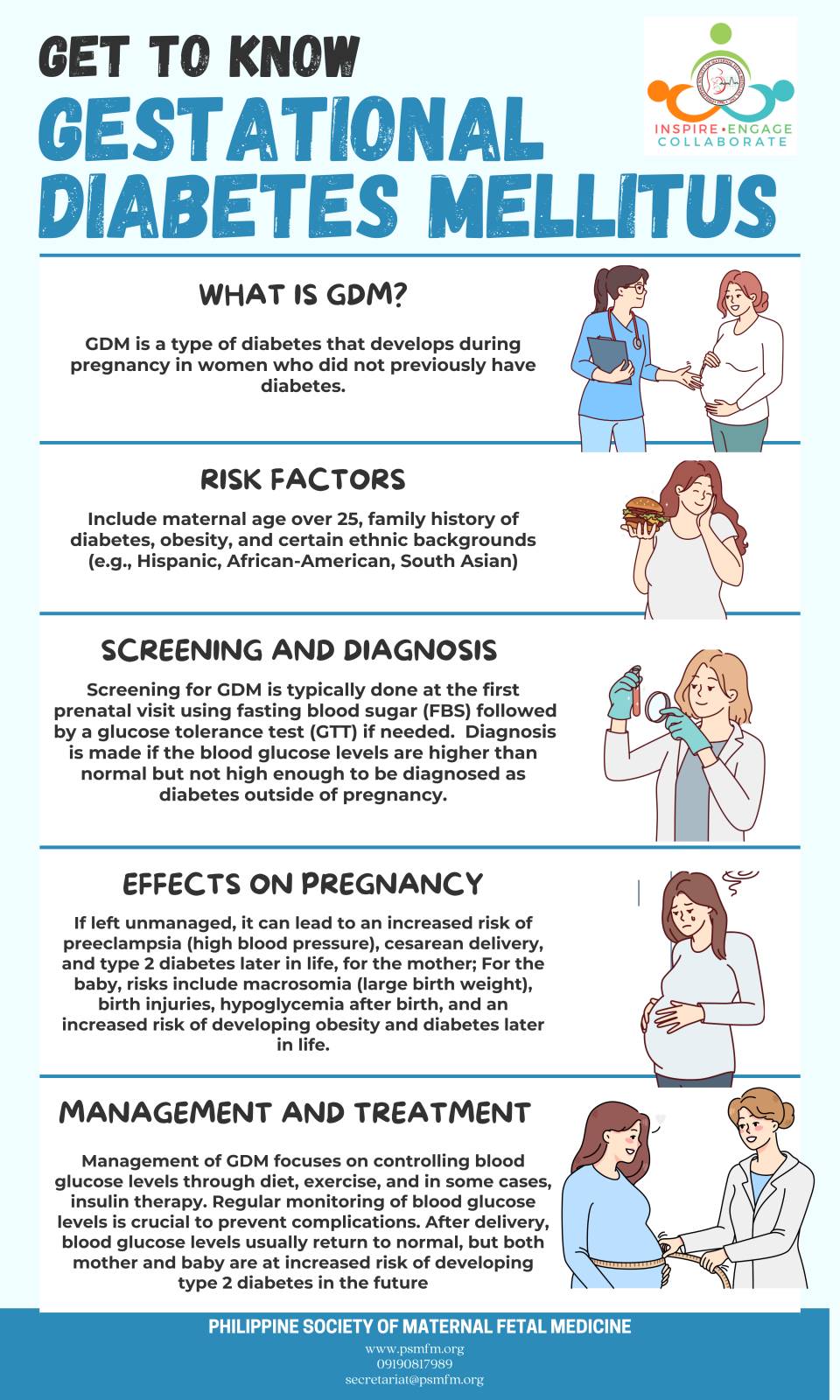
Gestational diabetes mellitus is a type of diabetes that develops only during pregnancy. Unlike type 1 or type 2 diabetes, GDM usually resolves after childbirth—but it requires careful management to protect both mom and baby.
Why does it happen?
During pregnancy, your placenta produces hormones that can cause insulin resistance. If your body can’t make enough insulin to overcome this resistance, blood sugar rises—leading to GDM.
“Gestational diabetes isn’t your fault,” says Dr. Sarah Johnson, OB-GYN and maternal-fetal medicine specialist at Mayo Clinic. “It’s a physiological response to pregnancy, not a reflection of lifestyle choices.”
While risk factors include being overweight, having a family history of diabetes, or being over 25, many women with no risk factors still develop GDM—including the patient in this story.
(Learn more about the medical definition on Wikipedia .)
The Day I Was Diagnosed: Shock, Fear, and Then Clarity
At 26 weeks pregnant, I failed my 1-hour glucose screening test. Two days later, I sat in a quiet exam room, staring at my hands as my doctor said, “Your 3-hour glucose tolerance test confirms gestational diabetes mellitus.”
My immediate thoughts:
- “Did I do something wrong?”
- “Will my baby be okay?”
- “Do I have to give up everything I love to eat?”
The truth? Emotional whiplash is normal. But within a week of working with a dietitian and endocrinologist, I realized: this was manageable—and even empowering.
How I Managed Gestational Diabetes: A Step-by-Step Plan That Worked
Here’s exactly what I did—backed by medical guidance and real-world trial and error:
1. Blood Sugar Monitoring (4x Daily)
- Fasting: <95 mg/dL
- 1 hour after meals: <140 mg/dL
- 2 hours after meals: <120 mg/dL
I used a contour next glucose meter and logged every reading in a free app (Glucose Buddy). Consistency was key—even on days I felt fine.
2. Meal Planning with a Registered Dietitian
My dietitian helped me build meals using the “plate method”:
- ½ plate non-starchy veggies (spinach, broccoli, zucchini)
- ¼ plate lean protein (chicken, tofu, eggs)
- ¼ plate complex carbs (quinoa, sweet potato, whole-grain bread)
Critical tip: Always pair carbs with protein or fat to blunt blood sugar spikes. Example: apple + almond butter, not apple alone.
3. Daily Movement—Even When Exhausted
- 10-minute walk after each meal (reduces post-meal glucose by up to 22%, per a 2020 Diabetes Care study)
- Prenatal yoga 3x/week
- Avoided sitting for >60 minutes at a time
4. Medication (When Diet & Exercise Weren’t Enough)
By week 32, my fasting numbers crept up. My doctor prescribed metformin—safe in pregnancy and far more effective than insulin for many women. I started with 500 mg once daily, increasing to 500 mg twice daily after 3 days.
“About 15–30% of women with GDM need medication,” notes the American College of Obstetricians and Gynecologists (ACOG).
What I Wish I’d Known Sooner
✅ Myth vs. Reality
| “You caused this by eating too much sugar.” | GDM is driven by pregnancy hormones—not candy. |
| “You’ll have diabetes for life.” | Most women’s blood sugar normalizes after delivery. |
| “You can’t eat any carbs.” | Youcan—just choose wisely and control portions. |
✅ Postpartum Follow-Up Is Non-Negotiable
I had a 2-hour oral glucose tolerance test at 6 weeks postpartum. Result: normal. But I now get screened for type 2 diabetes every 1–3 years—because women with GDM have a 50% higher risk of developing type 2 later in life (CDC).
Emotional & Social Challenges Nobody Talks About
- Guilt: “Am I harming my baby?” → Reality: Managing GDM reduces risks significantly.
- Isolation: Friends didn’t understand why I couldn’t share birthday cake → I learned to say, “My doctor has me on a special plan—thanks for understanding!”
- Anxiety: Constant monitoring felt obsessive → I scheduled “worry time” (10 minutes/day) to process fears, then shifted focus.
Support groups (like those on Beyond Type 1 or r/GestationalDiabetes on Reddit) made a huge difference.
FAQ: Your Top Questions About Gestational Diabetes
Q: Can gestational diabetes harm my baby?
A: If uncontrolled, yes—it can lead to macrosomia (large birth weight), preterm birth, or low blood sugar after delivery. But with proper management, most women deliver healthy babies.
Q: Will I need a C-section if I have GDM?
A: Not necessarily. Many women with GDM have vaginal deliveries. However, if the baby is very large (>9 lbs) or there are other complications, your provider may recommend a C-section.
Q: Can I prevent gestational diabetes in future pregnancies?
A: You can reduce risk by maintaining a healthy weight before pregnancy, staying active, and eating a balanced diet. But even then, GDM can still occur due to hormonal changes.
Q: Does gestational diabetes go away after birth?
A: Yes, in 90% of cases. However, you remain at higher risk for type 2 diabetes later—so regular screening is essential.
Q: What foods should I avoid completely?
A: Avoid sugary drinks (soda, juice), white bread/pasta, and desserts with added sugar. Focus on whole, fiber-rich foods instead.
Q: How often should I test my blood sugar?
A: Typically 4 times/day: fasting + 1–2 hours after breakfast, lunch, and dinner. Your care team will personalize this.
Conclusion: You’ve Got This
Hearing “you have gestational diabetes mellitus” might feel like a setback—but it’s really a call to action. With the right tools, support, and mindset, you can protect your health and your baby’s. My journey taught me resilience, self-advocacy, and the power of small daily choices.
If this story helped you, share it with someone who needs it. A single post could ease another mom’s fear or guide her to take that first blood sugar test without shame.
💬 Your turn: Have you experienced GDM? What tips would you add? Comment below or share on social media with #GDMJourney.
Leave a Reply