Being diagnosed with Type 1 diabetes changes everything—your routines, your mindset, even your relationship with food and your own body. If you or a loved one is navigating this condition, you’re not alone. Millions of Americans live with Type 1 diabetes, and understanding the patient experience Type 1 diabetes can empower you to manage it more effectively, reduce stress, and improve quality of life. This article shares real insights, expert-backed strategies, and practical tools based on lived experiences and clinical research.
What Is Type 1 Diabetes—and How Does It Affect Daily Life?
Type 1 diabetes (T1D) is an autoimmune condition where the pancreas produces little to no insulin—a hormone essential for regulating blood sugar. Unlike Type 2 diabetes, T1D isn’t caused by lifestyle factors and typically appears in childhood or adolescence, though adult-onset cases (LADA) do occur.
According to the Centers for Disease Control and Prevention (CDC), approximately 1.6 million Americans have Type 1 diabetes, including about 187,000 children and adolescents. Managing it requires constant vigilance: checking blood glucose, calculating insulin doses, monitoring diet, and preparing for emergencies like hypoglycemia.
“Every day with T1D is a balancing act,” says Dr. Jane Anderson, an endocrinologist at Johns Hopkins. “Patients aren’t just managing a disease—they’re managing life around a disease.”
For more background on the condition, see the Type 1 diabetes entry on Wikipedia .
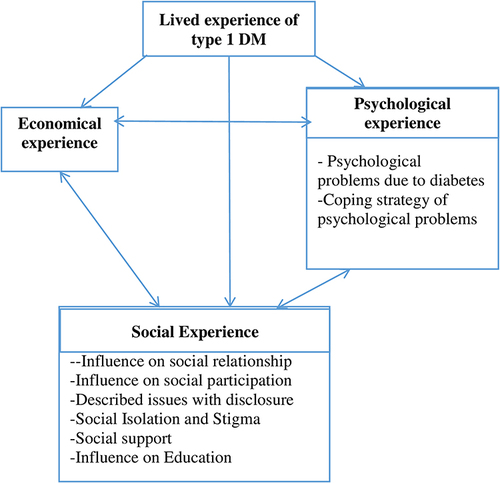
What Are the Biggest Challenges in the Patient Experience with Type 1 Diabetes?
Based on surveys from the T1D Exchange Registry and patient advocacy groups like Beyond Type 1, the top challenges include:
- Emotional burnout: Constant decision-making leads to “diabetes distress,” affecting 1 in 4 patients.
- Financial burden: Insulin prices in the U.S. remain high—some patients pay over $300/month out of pocket.
- Social stigma: Misconceptions (e.g., “Did you cause this by eating too much sugar?”) create isolation.
- Technology overload: While CGMs (continuous glucose monitors) and insulin pumps help, learning to use them adds complexity.
A 2023 study in Diabetes Care found that 68% of adults with T1D report anxiety about nighttime hypoglycemia, highlighting how fear impacts sleep and mental health.
How Can Patients Improve Their Daily Experience with Type 1 Diabetes?
Improving the patient experience Type 1 diabetes isn’t about perfection—it’s about sustainable, personalized strategies. Here’s a step-by-step approach:
1. Build a Support Ecosystem
- Join a local or online T1D community (e.g., Beyond Type 1 or JDRF forums).
- Involve family in education sessions—many clinics offer “diabetes school” for caregivers.
2. Optimize Technology Use
- Use a CGM (like Dexcom or Freestyle Libre) to reduce finger pricks and catch trends early.
- Pair with an insulin pump or automated insulin delivery (AID) system if eligible.
- Pro tip: Set glucose alerts at 70 mg/dL (low) and 180 mg/dL (high) as starting points—adjust based on your patterns.
3. Prioritize Mental Health
- Screen for diabetes distress using the PAID (Problem Areas in Diabetes) scale—available free online.
- Seek a therapist experienced in chronic illness (many accept telehealth).
4. Master Carb Counting—Without Obsession
- Start with consistent meals: e.g., 30g carbs for breakfast, 45g for lunch, 60g for dinner.
- Use apps like MyFitnessPal or Glucose Buddy to track and learn patterns.
5. Plan for Emergencies
- Always carry fast-acting glucose (e.g., 15g glucose tablets).
- Wear medical ID jewelry—911 responders check for it first.
Patient Experience: Real Stories That Inspire
Case Study: Maya, 28, Graphic Designer
Diagnosed at 12, Maya struggled with burnout in her 20s. After joining a peer support group and switching to a hybrid closed-loop pump, her A1C dropped from 8.9% to 6.7% in 6 months. “I stopped seeing diabetes as my enemy,” she says. “Now it’s just part of my toolkit.”
Case Study: James, 42, Teacher
James developed T1D at 38 (LADA). He felt isolated until he started a school-wide “Diabetes Awareness Week.” “Teaching others helped me accept it,” he shares. His students now know how to help if he goes low.
Traditional Care vs. Patient-Centered Care: What’s Better for T1D?
| Decision-Making | Doctor-led | Shared (patient + care team) |
| Visit Focus | A1C numbers | Holistic well-being (sleep, stress, goals) |
| Tech Integration | Optional | Built into treatment plan |
| Support Resources | Limited | Includes mental health, nutritionist, peer mentors |
Research shows patient-centered models reduce A1C by 0.5–1.0% on average and improve treatment adherence (per Journal of the American Medical Association, 2022).
FAQ: Patient Experience Type 1 Diabetes
Q: Can you live a normal life with Type 1 diabetes?
A: Absolutely. With modern tools and support, people with T1D run marathons, become pilots, and have healthy pregnancies. “Normal” looks different—but full, active lives are not only possible, they’re common.
Q: How often should I check my blood sugar?
A: It depends on your tech. With a CGM, you may never finger-prick. Without one, 4–10 times/day is typical—before meals, after exercise, at bedtime, and if you feel low.
Q: Is Type 1 diabetes genetic?
A: There’s a genetic component, but it’s not directly inherited like eye color. Having a parent with T1D raises risk slightly (about 5–10% if the father has it, 2–4% if the mother does), but most patients have no family history.
Q: What’s the biggest mistake new patients make?
A: Trying to be “perfect.” Blood sugar will fluctuate—it’s data, not failure. Focus on trends, not single numbers.
Q: How can I afford insulin and supplies?
A: Explore options:
- Manufacturer assistance programs (e.g., InsulinHelp.org)
- Walmart’s ReliOn insulin ($25/vial)
- Nonprofits like Insulin for Life USA
- Ask your doctor about biosimilar insulins (e.g., Semglee)
Q: Does stress really affect blood sugar?
A: Yes. Stress hormones like cortisol raise glucose levels. One study found exam week increased average glucose by 25 mg/dL in teens with T1D. Mindfulness, sleep, and routine help buffer this.
Conclusion
The patient experience Type 1 diabetes is deeply personal—but you don’t have to navigate it alone. From smart tech to emotional resilience and community support, there are proven ways to turn daily management into empowered living.
If this article helped you or someone you care about, share it on Facebook, Twitter, or Instagram—you might be the lifeline another person needs today.
Remember: You’re not defined by your diagnosis. You’re defined by how you rise with it. 💙
Leave a Reply