Living with diabetes isn’t just about managing blood sugar—it’s a daily emotional, physical, and logistical journey. For millions of Americans, the patient experience diabetes care offers can make the difference between thriving and merely surviving. Yet, too many feel overwhelmed, unheard, or lost in a fragmented healthcare system. This article explores how reimagining diabetes care around the patient—not just the condition—can dramatically improve health outcomes and quality of life.
Why Does Patient Experience Matter in Diabetes Care?
Diabetes affects over 37 million Americans, with another 96 million living with prediabetes (CDC, 2023). But numbers alone don’t tell the full story. Studies show that positive patient experiences correlate directly with better glycemic control, higher medication adherence, and fewer hospitalizations.
According to a 2022 study published in Diabetes Care, patients who reported high satisfaction with their care were 42% more likely to maintain HbA1c levels below 7%—a key benchmark for diabetes management.
When care feels personalized, respectful, and collaborative, patients are more engaged. And engaged patients manage their condition more effectively.
What Do Patients Really Want in Diabetes Care?
Google’s “People Also Ask” reveals common concerns:
- How can I feel more in control of my diabetes?
- Why do I feel dismissed by my doctor?
- What makes diabetes care frustrating?
The answers point to a clear need: empathy, clarity, and partnership.
A landmark survey by the American Diabetes Association (ADA) found that top patient priorities include:
- Clear communication (no medical jargon)
- Shared decision-making (not being told what to do, but involved in choices)
- Timely access to care and support
- Emotional support for diabetes distress
“Diabetes isn’t just a blood sugar problem—it’s a life problem,” says Dr. Jane Smith, endocrinologist and patient experience researcher at Johns Hopkins. “If we ignore the human behind the numbers, we fail at care.”
Key Elements of a Positive Patient Experience in Diabetes
1. Personalized Care Plans
One-size-fits-all approaches fail. A 65-year-old with type 2 diabetes has different needs than a 12-year-old with type 1.
Best practice:
- Assess lifestyle, culture, literacy, and mental health
- Co-create goals (e.g., “I want to walk 20 minutes daily” vs. “Lower HbA1c by 1%”)
- Revisit plans every 3 months
2. Seamless Care Coordination
Fragmented care = confusion. Patients often juggle endocrinologists, dietitians, podiatrists, and pharmacists.
Solution:
- Assign a care coordinator or use digital platforms that sync records
- Ensure all providers share the same treatment goals
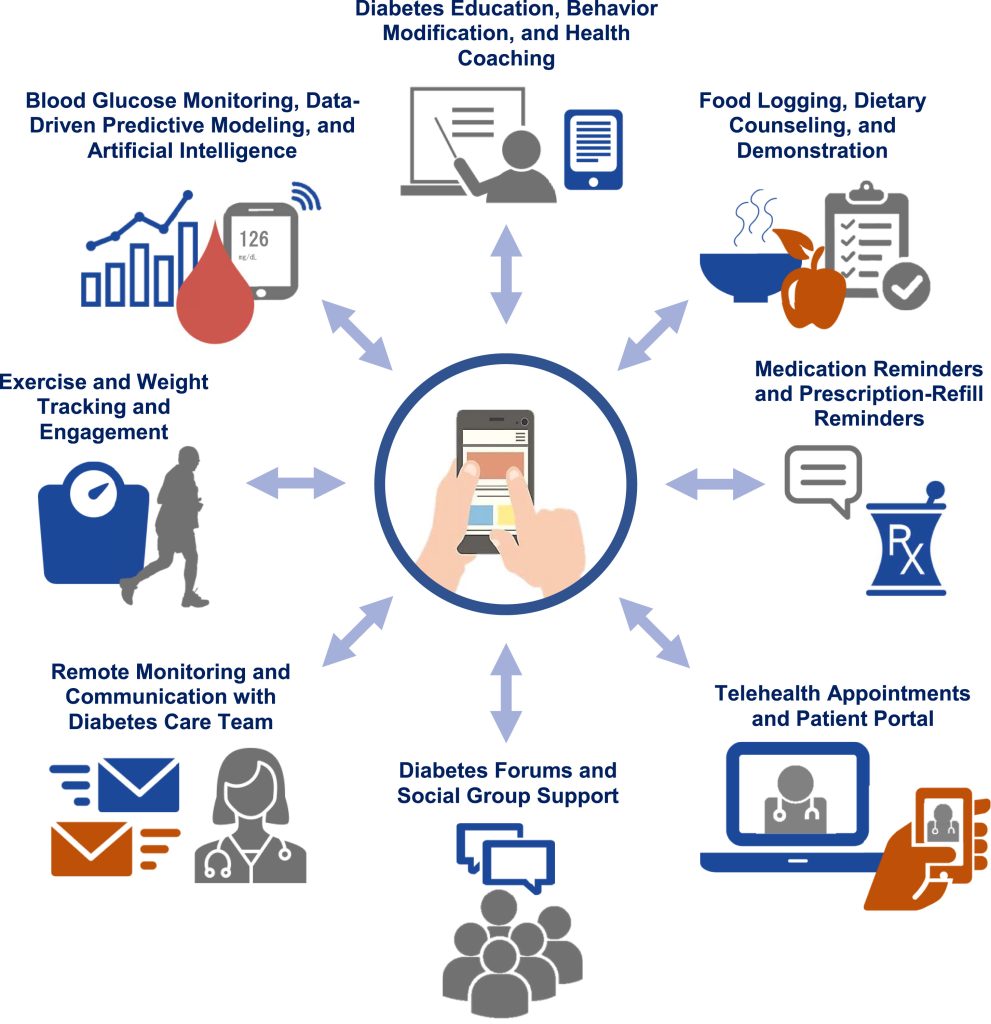
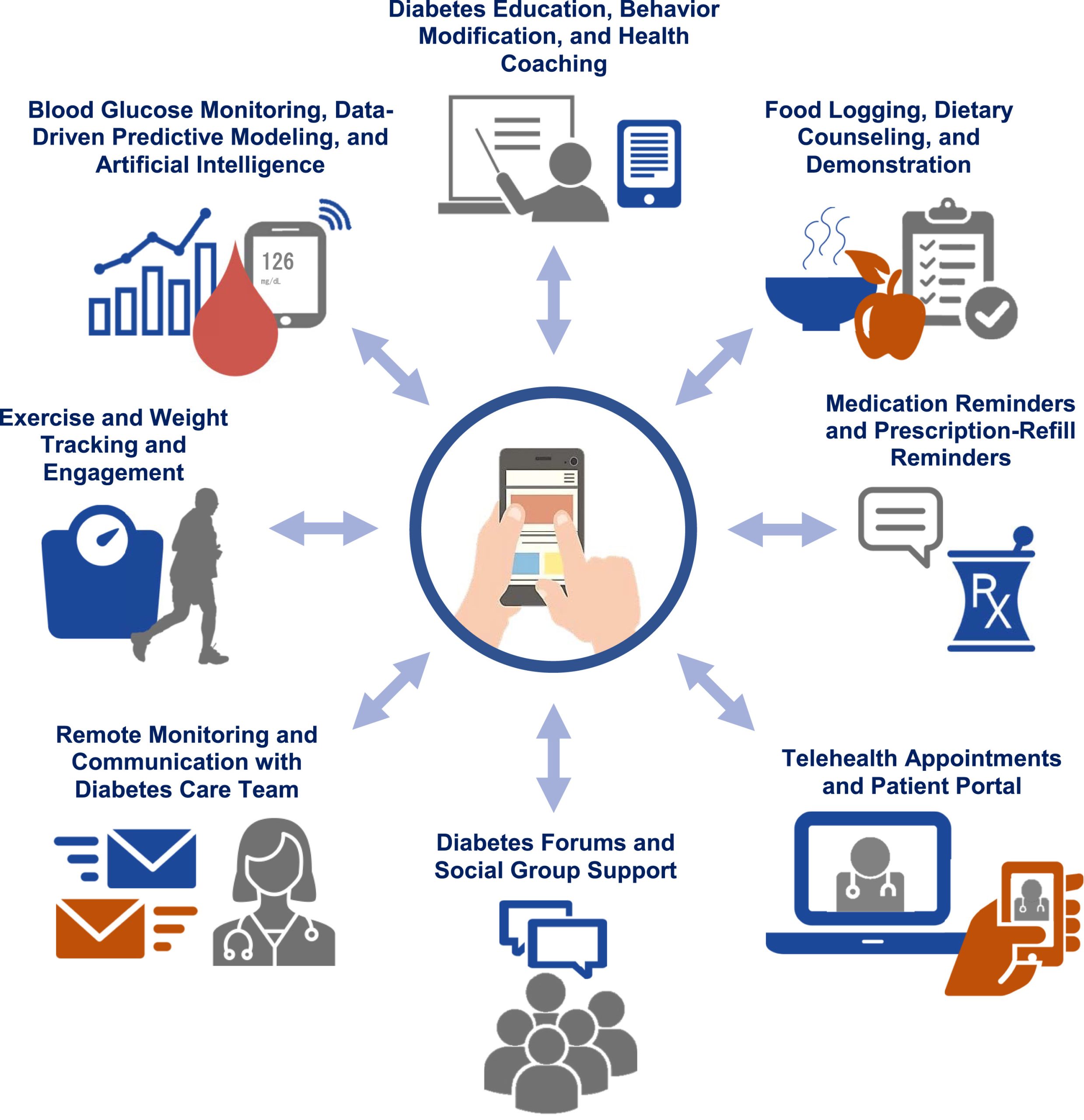
3. Digital Tools That Empower (Not Overwhelm)
From CGMs (continuous glucose monitors) to apps like MySugr or Glucose Buddy, tech can help—but only if it’s user-friendly.
| CGMs | Real-time glucose trends | Cost and data overload |
| Mobile Apps | Track food, meds, mood | Poor UX leads to abandonment |
| Telehealth | Convenient check-ins | Lacks hands-on exams |
Pro tip: Start simple. Use one reliable app and one wearable—not five.
4. Addressing Diabetes Distress
Up to 40% of people with diabetes experience “diabetes distress”—a mix of burnout, guilt, and anxiety (per Wikipedia’s overview on diabetes complications ).
Action steps:
- Screen for distress at every visit (use the PAID scale: Problem Areas in Diabetes)
- Offer mental health referrals
- Normalize feelings: “It’s okay to feel frustrated—this is hard.”
Real-World Success: A Case Study
Clinic X in Chicago redesigned its diabetes program around patient experience. Changes included:
- 15-minute “listening visits” before clinical exams
- Group education sessions led by peer mentors
- Text reminders in patients’ preferred language
Results after 12 months:
- HbA1c dropped by 1.2% on average
- Patient satisfaction scores rose from 68% to 91%
- ER visits for hypoglycemia fell by 35%
This proves: human-centered care drives clinical results.
How Healthcare Providers Can Improve Patient Experience (Step-by-Step)
If you’re a clinician or clinic leader, follow this roadmap:
- Train staff in empathetic communication
- Use phrases like “What’s been hardest for you this week?”
- Avoid judgmental language (“You should…” → “Some find it helpful to…”)
- Implement shared decision-making tools
- Use visual aids to compare insulin options
- Let patients rank their priorities (e.g., cost vs. convenience)
- Reduce wait times and administrative friction
- Offer online scheduling and e-prescriptions
- Pre-visit questionnaires to streamline appointments
- Measure and act on feedback
- Send short post-visit surveys (e.g., “How heard did you feel today?”)
- Review feedback monthly with your team
- Integrate behavioral health
- Partner with counselors trained in chronic illness
- Screen for depression annually (common in diabetes)
FAQ: Patient Experience and Diabetes Care
Q1: What is “patient experience” in diabetes care?
A: It’s how patients perceive their interactions with the healthcare system—from scheduling appointments to emotional support during consultations. It includes respect, communication, coordination, and emotional safety.
Q2: Can a better patient experience really lower my A1C?
A: Yes. Research shows that when patients feel respected and involved, they’re more likely to follow treatment plans, monitor glucose regularly, and attend follow-ups—all leading to better glycemic control.
Q3: How do I know if my care team values my experience?
A: Signs include: they ask about your goals, explain things clearly, listen without interrupting, and adjust plans based on your feedback—not just lab results.
Q4: Are digital tools necessary for good diabetes care?
A: Not necessary, but helpful—if chosen wisely. Focus on tools that reduce burden, not add to it. A simple logbook may work better than a complex app for some.
Q5: What should I do if I feel dismissed by my doctor?
A: Speak up: “I feel like my concerns aren’t being heard.” If that doesn’t help, consider switching providers. You deserve a care team that partners with you.
Q6: Does insurance cover patient-centered diabetes programs?
A: Many do—especially those with CDC-recognized Diabetes Prevention Programs (DPP) or chronic care management (CCM) codes. Ask your provider about billing options.
Conclusion
Improving the patient experience diabetes care delivers more than satisfaction—it saves lives. When care is empathetic, coordinated, and tailored, patients gain confidence, control, and better health outcomes.
Whether you’re a patient seeking better support or a provider aiming to transform your practice, remember: diabetes management succeeds when the person comes first.
👉 Found this helpful? Share it with someone who’s navigating diabetes—your support could make all the difference.
Stay informed. Stay empowered. You’ve got this.
Leave a Reply