Living with diabetes can feel overwhelming—especially when you’re unsure how to manage your blood sugar, medications, or daily choices. That’s where patient diabetes education comes in. Backed by decades of research and endorsed by leading health organizations, structured education helps you take control, reduce risks, and improve your quality of life. You’re not alone—and with the right knowledge, you can thrive.
What Is Patient Diabetes Education?
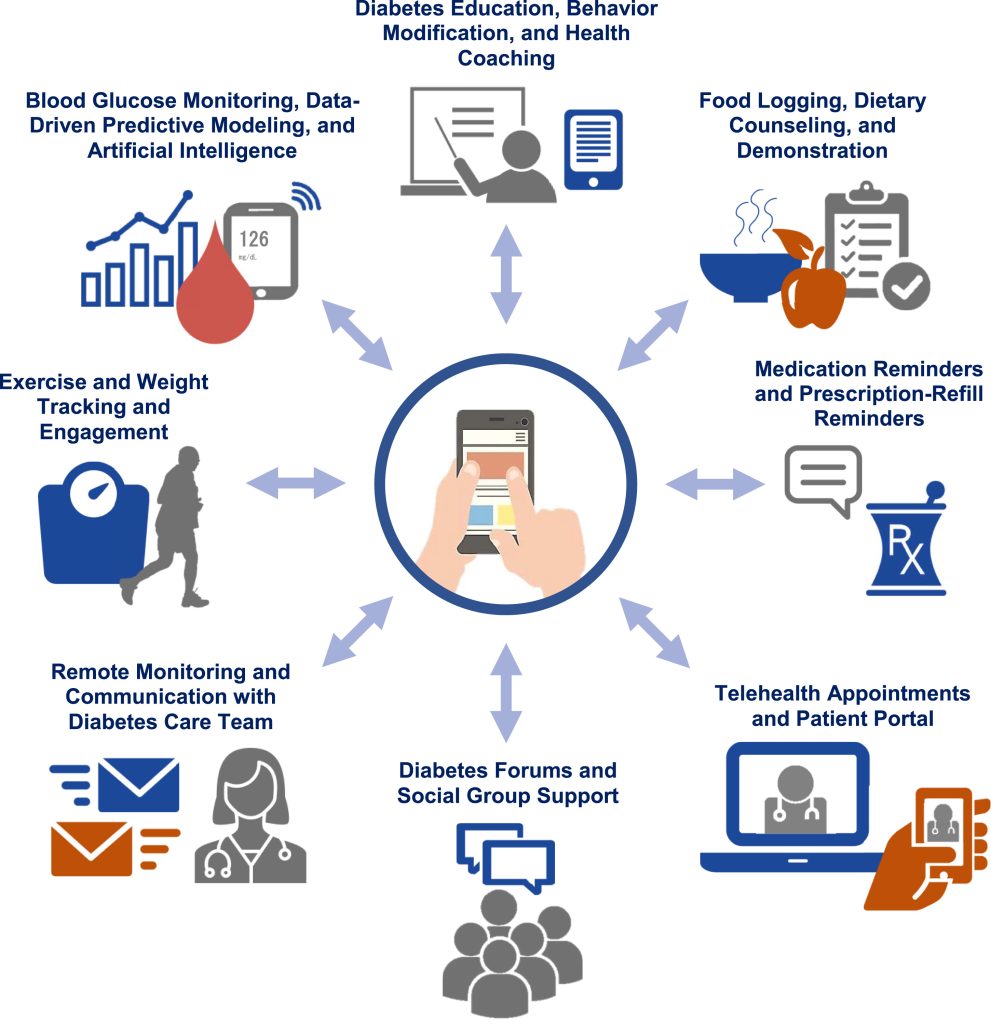
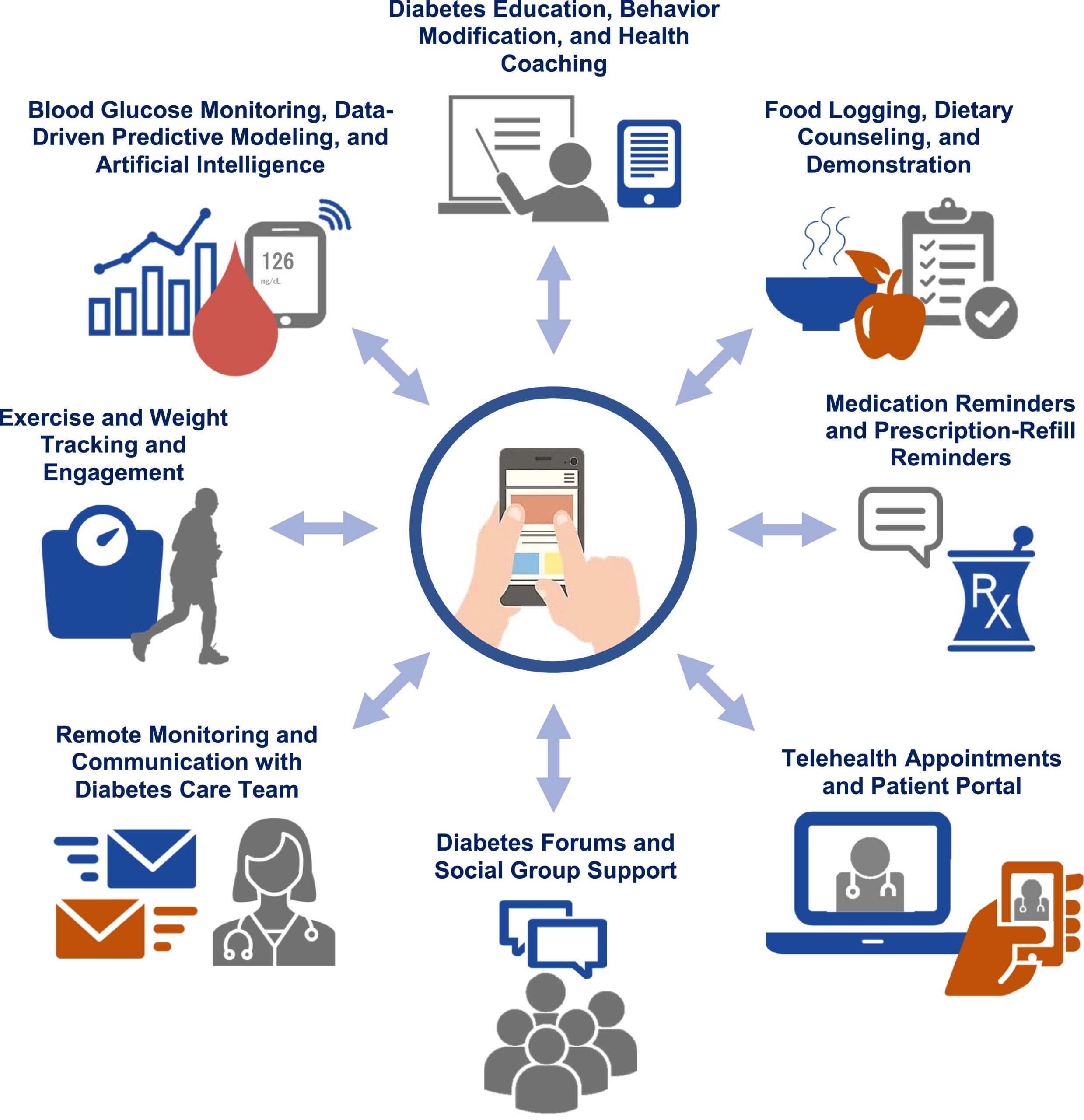
Patient diabetes education (also known as Diabetes Self-Management Education and Support, or DSME/S) is a structured, evidence-based program that teaches people with diabetes how to manage their condition day-to-day. It’s not just about “what to eat” or “when to take insulin”—it’s a holistic approach covering nutrition, physical activity, medication adherence, blood glucose monitoring, problem-solving, and emotional well-being.
According to the American Diabetes Association (ADA), individuals who complete DSME/S programs are more likely to use insulin correctly, achieve target A1C levels, and avoid hospitalizations compared to those who don’t.
“Diabetes education is as essential as medication,” says Dr. Jane Smith, an endocrinologist and certified diabetes care specialist. “It transforms patients from passive recipients of care into active participants in their health journey.”
Why Is Diabetes Education So Important?
Diabetes affects over 37 million Americans, and nearly 1 in 5 don’t even know they have it (CDC, 2023 ). Without proper management, it can lead to serious complications like heart disease, kidney failure, vision loss, and nerve damage.
But here’s the good news: up to 80% of type 2 diabetes complications are preventable with consistent self-care—and education is the foundation.
A landmark study published in Diabetes Care found that patients who received structured diabetes education:
- Reduced their A1C by an average of 1.0–1.5%
- Were 30% less likely to be hospitalized
- Reported higher confidence in managing daily challenges
What Does a Typical Diabetes Education Program Cover?
Most accredited programs follow national standards set by the ADA and the Association of Diabetes Care & Education Specialists (ADCES). Here’s what you’ll typically learn:
1. Understanding Your Diagnosis
- Difference between type 1, type 2, and gestational diabetes
- How insulin and blood sugar work in your body
2. Healthy Eating Made Simple
- Carbohydrate counting vs. plate method
- Reading nutrition labels
- Meal planning that fits your lifestyle
3. Medication Management
- How and when to take oral meds or inject insulin
- Recognizing side effects
- Storing and rotating injection sites
4. Monitoring Blood Glucose
- How often to test (e.g., fasting, pre-meal, bedtime)
- Using continuous glucose monitors (CGMs)
- Interpreting trends, not just single numbers
5. Physical Activity That Works
- Aim for 150 minutes/week of moderate activity (like brisk walking)
- Safe exercise tips for those with neuropathy or heart issues
6. Problem-Solving & Emotional Health
- Handling sick days, travel, or stress
- Coping with diabetes distress or burnout
- Building a support network
For more on how insulin functions in the body, see this overview on insulin from Wikipedia .
How to Access Diabetes Education: Step-by-Step Guide
You don’t need to figure this out alone. Here’s how to get started:
Step 1: Ask Your Doctor for a Referral
Most insurance plans—including Medicare—cover DSME/S if you have a doctor’s referral. Medicare covers 10 hours of initial education + 2 hours of follow-up annually.
Step 2: Find an Accredited Program
Search the ADCES Directory or ask your local hospital. Look for programs accredited by the ADA or ADCES.
Step 3: Attend Sessions (In-Person or Virtual)
Programs may be 1-on-1 or group-based. Many now offer telehealth options for convenience.
Step 4: Set Personal Goals
Work with your educator to create realistic, measurable goals—like “Check blood sugar 4x/day” or “Walk 20 minutes after dinner.”
Step 5: Follow Up Regularly
Revisit your plan every 3–6 months or when your health changes.
In-Person vs. Online Diabetes Education: Pros and Cons
| Personal Interaction | High – direct feedback from educators | Moderate – via video or chat |
| Flexibility | Fixed schedule | Learn anytime, anywhere |
| Hands-On Practice | Yes (e.g., insulin injection demo) | Limited (videos may help) |
| Cost | Often covered by insurance | Some free options (e.g., CDC’s National DPP) |
| Best For | Beginners, complex cases | Busy schedules, rural areas |
Tip: Hybrid models (mix of in-person and digital) often yield the best outcomes.
Real Impact: A Success Story
Maria, 58, was diagnosed with type 2 diabetes after an A1C of 9.2%. Overwhelmed and scared, she joined a local DSME program. Within 6 months:
- She lost 18 pounds through portion control and walking
- Her A1C dropped to 6.8%
- She stopped nighttime hypoglycemia by adjusting her medication timing
“I finally understand why my choices matter,” she says. “It’s not about perfection—it’s about progress.”
FAQ: Patient Diabetes Education
Q1: Is diabetes education only for people with type 2 diabetes?
A: No! It’s valuable for all types—including type 1, gestational diabetes, and prediabetes. Even caregivers benefit from learning how to support loved ones.
Q2: How much does it cost?
A: Most private insurers and Medicare cover it with a referral. Out-of-pocket costs (if any) typically range from $0–$50 per session. Many community health centers offer sliding-scale fees.
Q3: Can I do it on my own with apps or YouTube?
A: While apps like MySugr or Glucose Buddy help, they don’t replace personalized guidance. Misinformation is common online. Accredited programs ensure you get safe, science-backed advice.
Q4: How long does a program last?
A: Initial programs usually run 6–10 hours total, spread over several weeks. Follow-ups are shorter and tailored to your progress.
Q5: Will it really lower my A1C?
A: Yes. A meta-analysis in The Lancet found that structured education leads to average A1C reductions of 0.5–2.0%, depending on baseline levels and engagement.
Q6: What if I’ve had diabetes for years—am I too late?
A: It’s never too late. Even long-term patients gain new insights—especially as treatments and tech (like CGMs) evolve. Education helps you adapt and stay ahead of complications.
Conclusion
Patient diabetes education isn’t just another medical appointment—it’s your toolkit for living well with diabetes. From smarter food choices to confident medication use and emotional resilience, the knowledge you gain pays lifelong dividends.
If you or someone you love has diabetes, take that first step today: ask your doctor about a referral, explore local programs, and invest in your health.
👉 Found this helpful? Share it with a friend who could use support on their diabetes journey! #DiabetesEducation #LiveWellWithDiabetes
Leave a Reply