If you or a loved one is hospitalized with diabetes, you’re not alone—over 37 million Americans live with diabetes, and many require hospitalization each year for related or unrelated conditions. Managing blood sugar in the hospital is complex, but in-patient diabetes care is critical to preventing complications like infections, delayed healing, or even life-threatening events. This guide explains how hospitals deliver safe, evidence-based care—and what you can expect during a stay.
What Is In-Patient Diabetes Care?
In-patient diabetes care refers to the specialized medical management of blood glucose levels for patients admitted to a hospital. Unlike outpatient care, which focuses on long-term control, in-patient care prioritizes acute stabilization, prevention of hypo- or hyperglycemia, and coordination across multiple care teams.
According to the American Diabetes Association (ADA), up to 38% of hospitalized patients have diabetes or hyperglycemia, yet many hospitals still face challenges in consistent glucose management. That’s why structured protocols—like basal-bolus insulin regimens—are now standard in high-performing facilities.
💡 Did you know? Poor glycemic control during hospitalization increases the risk of readmission by 27% (Journal of Hospital Medicine, 2022).
Why Is Blood Sugar Control So Critical in the Hospital?
When you’re sick or recovering from surgery, stress hormones like cortisol and adrenaline spike—raising blood glucose even in non-diabetics. For people with diabetes, this can lead to dangerous highs (hyperglycemia) or sudden drops (hypoglycemia), both linked to worse outcomes.
Key risks of uncontrolled glucose in-hospital include:
- Longer hospital stays
- Higher infection rates (e.g., UTIs, surgical site infections)
- Increased risk of ICU admission
- Greater mortality risk, especially in cardiac or critically ill patients
The ADA recommends target glucose ranges of 140–180 mg/dL for most hospitalized patients, balancing safety and efficacy.
How Do Hospitals Manage Diabetes During Admission?
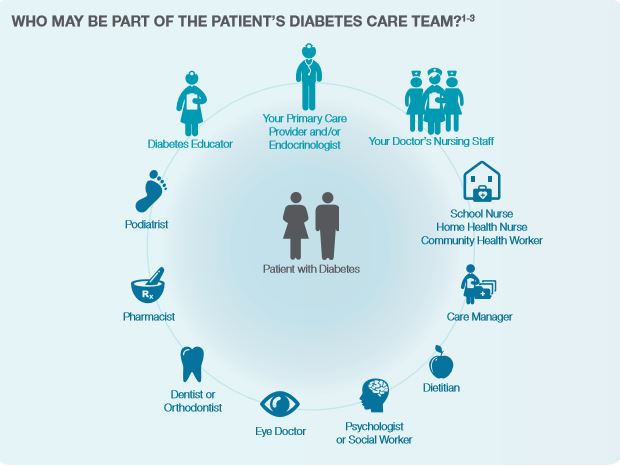
Modern in-patient diabetes care follows a multidisciplinary, protocol-driven approach. Here’s how it typically works:
1. Initial Assessment & Risk Stratification
Upon admission, nurses and endocrinologists evaluate:
- Type of diabetes (Type 1, Type 2, or steroid-induced)
- Current medications (e.g., insulin, SGLT2 inhibitors)
- Kidney function, nutritional status, and reason for hospitalization
⚠️ Note: Oral diabetes meds like metformin are often paused during hospitalization due to risks like lactic acidosis or dehydration.
2. Insulin Therapy: The Gold Standard
Most hospitals use basal-bolus insulin regimens instead of sliding scale alone, which is now considered outdated.
| Basal(e.g., glargine) | Controls fasting glucose | Once daily, usually at bedtime |
| Bolus(e.g., lispro) | Covers meals | 15–30 min before each meal |
| Correction | Treats high readings | As needed, based on protocol |
This approach mimics natural insulin release and reduces hypoglycemia risk by up to 50% compared to sliding scale (ADA Standards of Care, 2024).
3. Frequent Glucose Monitoring
- Non-critically ill patients: Blood glucose checked before meals and at bedtime (4x/day).
- ICU patients: Continuous glucose monitoring (CGM) or hourly checks via arterial line.
Newer hospitals are piloting real-time CGM systems (like Dexcom) even for in-patients, improving safety and reducing finger pricks.
4. Nutrition Coordination
Dietitians tailor meal plans to match insulin dosing. For example:
- Consistent carbohydrate meals (e.g., 45–60g carbs per meal)
- NPO (nothing by mouth) adjustments: Basal insulin continues, but bolus is held
Common Challenges in In-Patient Diabetes Care
Despite best efforts, hospitals face real-world hurdles:
| Staff knowledge gaps | Inconsistent insulin dosing | Mandatory diabetes education for nurses |
| Medication errors | Hypoglycemia events | Electronic health record (EHR) alerts |
| Discharge planning delays | Readmissions | Early involvement of diabetes educators |
| Steroid-induced hyperglycemia | Unpredictable spikes | Proactive insulin titration protocols |
A 2023 study in Diabetes Care found that hospitals using standardized order sets reduced severe hypoglycemia (<40 mg/dL) by 62% within one year.
For more on the pathophysiology and classification of diabetes, see the Wikipedia entry on diabetes mellitus .
Best Practices for Patients & Families
You’re not just a passive recipient—you can actively support safe care:
- Bring your medication list – Include insulin types, doses, and devices (pump, CGM).
- Ask about the glucose target – “What range are you aiming for during my stay?”
- Report symptoms – Sweating, shaking, or confusion could signal low blood sugar.
- Request a diabetes educator – Many hospitals offer bedside counseling.
✅ Pro tip: If you use an insulin pump or CGM, ask if the hospital allows continued use—some now support “hybrid” care models.
FAQ: In-Patient Diabetes Care
Q1: Can I keep using my insulin pump in the hospital?
A: It depends on the hospital’s policy and your condition. Many academic medical centers now permit pump use for stable patients, especially if you’re experienced. However, in critical care or during procedures, you may be switched to IV or subcutaneous insulin for safety.
Q2: Why was my metformin stopped during my hospital stay?
A: Metformin is often paused due to risks of lactic acidosis if you become dehydrated, have kidney issues, or undergo contrast imaging. It’s usually restarted before discharge if kidney function is normal.
Q3: What’s the difference between sliding scale and basal-bolus insulin?
A: Sliding scale only corrects high blood sugar after it happens (reactive), while basal-bolus prevents highs by providing background insulin (basal) plus meal coverage (bolus). Basal-bolus is strongly preferred by the ADA.
Q4: How often will my blood sugar be checked?
A: Typically 4 times daily (before meals and bedtime) for general wards. In the ICU, it may be hourly or via continuous monitoring.
Q5: Will my diabetes get worse after hospitalization?
A: Stress and medications (like steroids) can temporarily worsen control, but this often improves post-discharge. Follow up with your endocrinologist within 7–14 days to adjust your regimen.
Q6: Are there special protocols for surgery patients with diabetes?
A: Yes. Surgical teams use perioperative glycemic protocols, often involving IV insulin infusions during procedures and tight targets (100–150 mg/dL) to reduce infection risk.
Conclusion
In-patient diabetes care isn’t just about insulin—it’s a coordinated system designed to keep you safe, prevent complications, and support recovery. With evidence-based protocols, multidisciplinary teams, and growing use of technology like CGMs, hospitals are better equipped than ever to manage diabetes during admission.
If you found this guide helpful, share it with a friend or family member who might be facing a hospital stay. Knowledge is power—and when it comes to diabetes in the hospital, it can literally save lives. 💙
Leave a Reply