You’re Not Alone — And You’ve Got This
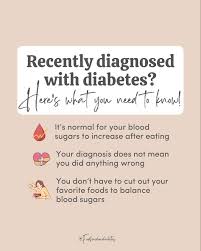
If you’re reading this, chances are you just heard the words: “You have diabetes.” It’s okay to feel overwhelmed, scared, or even numb. I was recently diagnosed with diabetes — and so have over 37 million Americans, according to the CDC. But here’s the truth: with the right knowledge and support, you can live a full, vibrant, healthy life. This guide is your first step forward — written with empathy, backed by science, and designed to help you take control, starting today.
What Does “I Was Recently Diagnosed With Diabetes” Really Mean?
First, let’s demystify the diagnosis. Diabetes isn’t a death sentence — it’s a metabolic condition where your body struggles to manage blood sugar (glucose). There are three main types:
Type 1 Diabetes: Your immune system attacks insulin-producing cells. Usually diagnosed in childhood or young adulthood.
Type 2 Diabetes: Your body becomes resistant to insulin or doesn’t make enough. Most common — 90–95% of cases.
Gestational Diabetes: Occurs during pregnancy and often resolves after birth.
Since you’re reading this, you likely have Type 2 — and that’s good news. Why? Because Type 2 diabetes is often reversible or highly manageable with lifestyle changes.
💡 According to the American Diabetes Association, losing just 5–7% of your body weight can reduce your risk of developing serious complications by over 58%.
What Should I Do First After My Diagnosis?
Take a deep breath. Then, follow these 5 immediate steps:
- Schedule a Follow-Up With Your Doctor
Don’t leave the office without a clear action plan. Ask:
What’s my A1C level? (Goal: under 7% for most adults)
Do I need medication? (Metformin is often first-line)
When’s my next check-up?
- Get a Blood Glucose Monitor
You’ll need to track your levels. Popular options:
OneTouch Verio Flex (user-friendly, color-coded results)
Dexcom G7 (continuous glucose monitor — CGM)
👉 Test before meals and 2 hours after eating. Target range: 80–130 mg/dL before meals, under 180 mg/dL after.
- Meet With a Certified Diabetes Care and Education Specialist (CDCES)
These pros help you build a personalized plan. Find one near you at diabeteseducator.org . - Clean Out Your Pantry
Remove or limit:
Sugary drinks (soda, juice, sweet tea)
White bread, pasta, and rice
Packaged snacks high in refined carbs
Stock up on:
Non-starchy veggies (spinach, broccoli, zucchini)
Lean proteins (chicken, fish, tofu)
Healthy fats (avocado, nuts, olive oil)
- Start Moving — Even Just 10 Minutes a Day
Walking after meals can lower blood sugar by up to 22%, per a 2016 study in Diabetologia. Aim for 150 minutes of moderate activity weekly — that’s just 22 minutes a day.
What Foods Should I Eat (and Avoid)?
Let’s make this simple. Think of your plate like this:
SECTION
WHAT TO FILL IT WITH
EXAMPLES
½ Plate
Non-starchy vegetables
Spinach, peppers, cauliflower
¼ Plate
Lean protein
Grilled salmon, tofu, skinless chicken
¼ Plate
Complex carbs or whole grains
Quinoa, brown rice, sweet potato
Foods to Limit or Avoid:
🚫 White bread, bagels, pastries
🚫 Sugary cereals and flavored yogurts
🚫 Fruit juice and soda (even “diet” versions can trigger cravings)
🚫 Processed meats (bacon, sausage, deli meats)
🌾 Swap white rice for cauliflower rice. Replace pasta with zucchini noodles. Small swaps = big blood sugar wins.
How Can I Lower My Blood Sugar Naturally?
You don’t need drastic changes. Start here:
✅ Hydrate Smart
Drink 8–10 glasses of water daily. Dehydration raises blood sugar.
✅ Prioritize Sleep
Aim for 7–9 hours. Poor sleep = higher insulin resistance.
✅ Manage Stress
Cortisol (the stress hormone) spikes glucose. Try:
5-minute deep breathing (inhale 4 sec, hold 4, exhale 6)
Daily walks in nature
Journaling for 10 minutes before bed
✅ Add Cinnamon or Apple Cider Vinegar
1 tsp cinnamon daily may lower fasting glucose by 10–29% (Journal of the Academy of Nutrition and Dietetics).
1 tbsp apple cider vinegar in water before meals can reduce post-meal spikes.
What Medications Might I Need?
Not everyone needs meds right away — but many do. Common prescriptions:
MEDICATION
HOW IT WORKS
COMMON SIDE EFFECTS
Metformin
Reduces liver glucose production
Mild stomach upset, diarrhea
GLP-1 Agonists (e.g., Ozempic)
Slows digestion, increases insulin
Nausea, reduced appetite
SGLT2 Inhibitors (e.g., Jardiance)
Helps kidneys remove sugar via urine
UTIs, yeast infections
💊 Always take meds as prescribed — even if you “feel fine.” Diabetes is often silent until damage is done.
Can I Reverse My Diabetes?
Yes — especially if you act early.
A landmark 2017 UK study (DiRECT trial) showed that 46% of participants reversed Type 2 diabetes after losing 15 kg (33 lbs) through a structured low-calorie diet and support.
Steps to Reversal:
Lose 10–15% of your body weight.
Exercise 30 mins/day, 5 days/week.
Eat whole, unprocessed foods.
Monitor blood sugar weekly.
Work with your care team — don’t go solo.
⏳ Reversal isn’t overnight — but every 1% drop in A1C reduces your risk of complications by 40% (per ADA).
What Are the Long-Term Risks If I Don’t Manage It?
Ignoring diabetes can lead to:
Heart disease (2–4x higher risk)
Kidney failure
Vision loss or blindness
Nerve damage (neuropathy)
Amputations
But — and this is critical — these are NOT inevitable. With daily management, you can avoid nearly all complications.
📊 The CDC reports that people who manage their A1C under 7% cut their risk of eye, kidney, and nerve disease by 40%.
Real Story: Maria’s Turnaround
Maria, 52, was diagnosed with an A1C of 9.1%. She felt defeated — until she joined a CDC-recognized lifestyle change program.
Swapped soda for sparkling water with lemon
Walked 20 minutes after dinner with her husband
Started meal prepping on Sundays
In 6 months, her A1C dropped to 6.2 — without medication. She’s now off her blood pressure meds too.
“I thought my life was over. Turns out, it was just beginning.” — Maria R., Ohio
FAQ: I Was Recently Diagnosed With Diabetes — Your Top Questions Answered
Q1: Is diabetes my fault?
A: Absolutely not. While lifestyle plays a role, genetics, age, stress, and even environmental toxins contribute. Blaming yourself helps no one. Focus on what you can control — starting now.
Q2: Can I still eat fruit?
A: Yes! Stick to low-glycemic fruits like berries, apples, and pears. Avoid fruit juice. Pair fruit with protein (like nuts) to slow sugar absorption.
Q3: How often should I check my blood sugar?
A: Depends on your treatment. If you’re on insulin: 2–4x/day. If not: your doctor may recommend fasting + 2 hours after meals, 2–3x/week. Always follow your care plan.
Q4: Will I need insulin?
A: Not necessarily. Many manage with diet, exercise, and oral meds. Insulin is safe and effective if needed — it’s not a “last resort.”
Q5: Can stress really affect my blood sugar?
A: Yes. Stress hormones like cortisol tell your liver to release more glucose — even if you haven’t eaten. That’s why mindfulness and sleep matter as much as diet.
Q6: Where can I find reliable info?
A: Start with trusted sources like the American Diabetes Association or Wikipedia’s diabetes page for foundational knowledge. Avoid social media “cures.”
You’ve Got a New Normal — And It Can Be Better Than Before
Hearing “I was recently diagnosed with diabetes” might feel like a door closing. But it’s actually a window opening — to better health, more energy, and deeper self-care than ever before.
You don’t have to be perfect. You just have to start. One meal. One walk. One blood sugar check at a time.
✅ You now have a roadmap.
✅ You’re not alone.
✅ Your future is still bright — maybe even brighter.
👉 Loved this guide? Share it with someone who needs hope today.
Tag a friend. Post it on Facebook. Save it for later. Let’s turn fear into action — together.
Because diabetes doesn’t define you. How you rise to meet it? That’s your story.
Leave a Reply