Explaining diabetes to a patient can feel overwhelming — whether you’re a healthcare provider, a caregiver, or even a loved one. The medical terms, the lifelong implications, the fear of needles or diet changes… it’s a lot. But here’s the good news: you don’t need to be a specialist to explain diabetes to a patient in a way that’s compassionate, clear, and empowering. In this guide, we’ll walk you through exactly how to do it — step by step — using plain language, visual analogies, and proven communication techniques trusted by endocrinologists and diabetes educators nationwide. Let’s turn confusion into confidence — together.
Why Explaining Diabetes Clearly Matters
According to the CDC, over 37 million Americans have diabetes — and 1 in 5 don’t even know it. Even among diagnosed patients, studies show that less than half fully understand how their condition works or how to manage it daily.
“The biggest barrier to diabetes control isn’t insulin or medication — it’s understanding.”
— Dr. Anne Peters, Director of USC Clinical Diabetes Programs
Misunderstanding leads to poor adherence, higher A1C levels, and preventable complications. That’s why how you explain diabetes to a patient is just as critical as the treatment plan itself.
Step-by-Step: How to Explain Diabetes to a Patient (Without Overwhelming Them)
Step 1: Start With the Big Picture — Use a Simple Analogy
Avoid: “Your pancreas doesn’t produce enough insulin due to beta-cell dysfunction…”
Try this instead:
“Think of your body like a car. Food is the fuel. Insulin is the key that unlocks your cells so the fuel can get in and give you energy. With diabetes, either your body lost the key (Type 1), or the lock is rusty and doesn’t work well (Type 2). So the fuel — sugar — builds up in your blood instead of powering you.”
This analogy is used by the American Diabetes Association (ADA) in patient education materials because it’s memorable, non-threatening, and accurate.
Step 2: Differentiate Type 1 vs Type 2 — Without Confusion
Many patients mix them up. Clarify with a simple table:
| Cause | Autoimmune — body attacks insulin cells | Insulin resistance + gradual insulin loss |
| Onset | Usually sudden, often in childhood | Gradual, often in adulthood |
| Treatment | Insulin injections or pump required | Diet, exercise, pills, sometimes insulin |
| Preventable? | No | Often yes, with lifestyle changes |
| % of Cases | ~5-10% | ~90-95% |
Source: American Diabetes Association
💡 Pro Tip: Say, “Type 1 is like being born without a key. Type 2 is like having a key that doesn’t turn smoothly anymore.”
Step 3: Explain Blood Sugar — But Make It Relatable
Don’t say: “Your glucose levels are elevated.”
Say:
“Imagine your bloodstream is a highway. Sugar (glucose) is the traffic. Too much traffic = traffic jam = damage to roads (your blood vessels). We want to keep traffic flowing smoothly — not too little, not too much.”
Use numbers they can visualize:
- Normal fasting blood sugar: 70–99 mg/dL → “Green zone”
- Prediabetes: 100–125 mg/dL → “Yellow zone — time to slow down”
- Diabetes range: 126+ mg/dL → “Red zone — needs action”
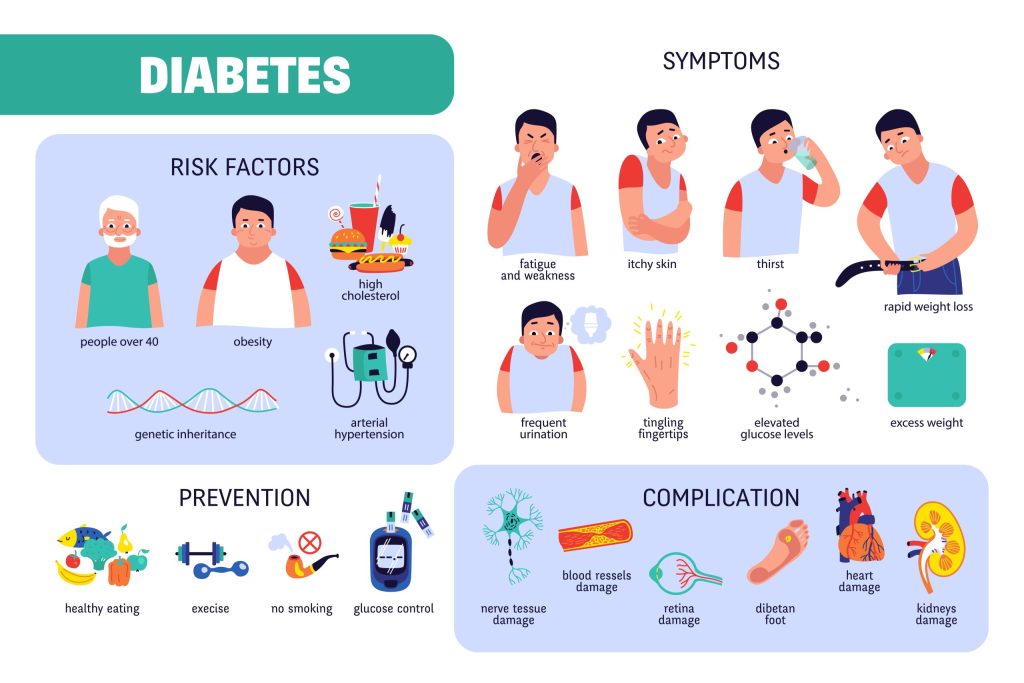
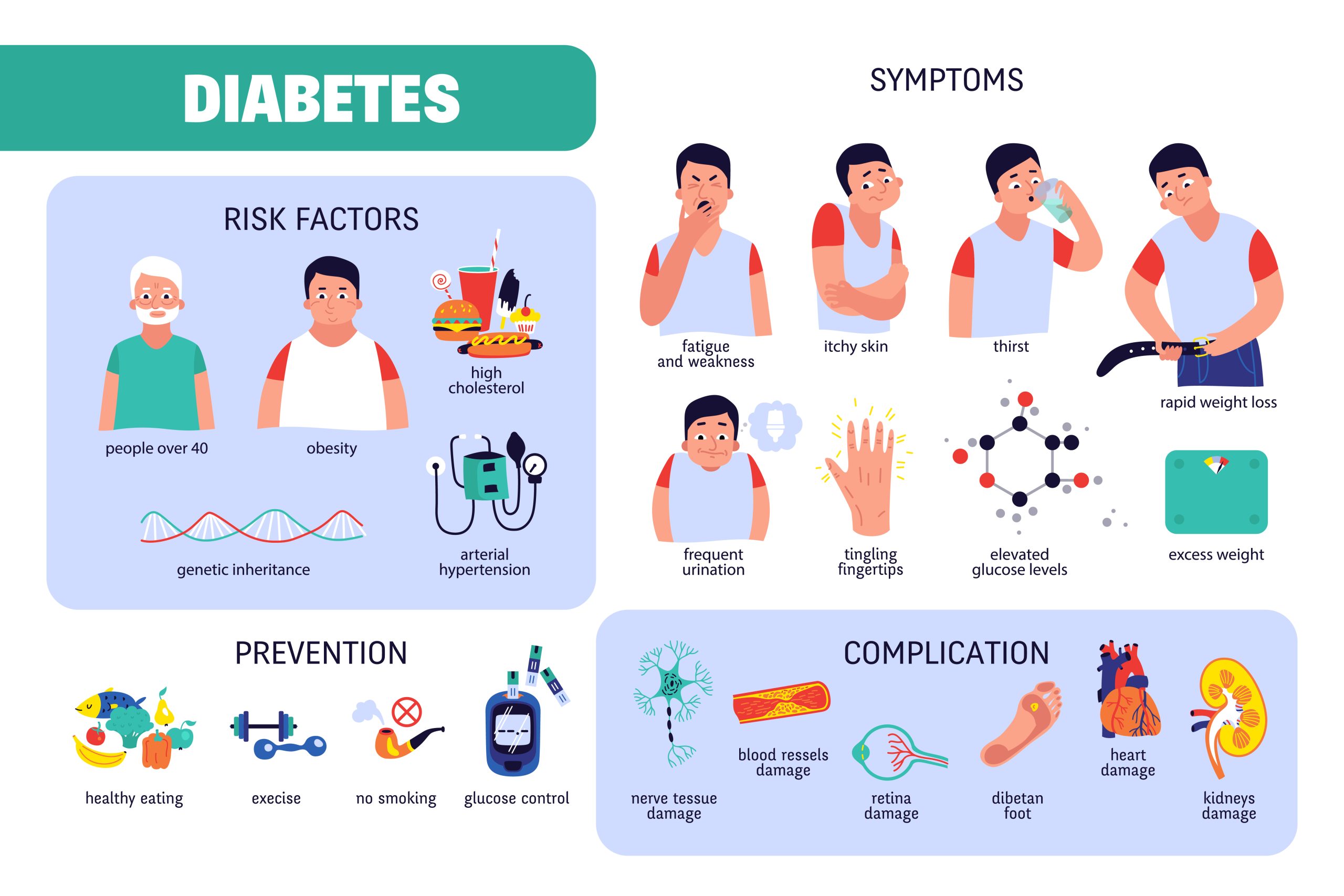
Step 4: Talk About Symptoms — But Frame Them as “Clues,” Not Scare Tactics
Instead of listing scary complications, say:
“Your body gives you clues when sugar is too high or too low. Let’s learn to read them — like a detective!”
High Blood Sugar Clues (Hyperglycemia):
- Always thirsty 🥤
- Peeing a lot 🚽
- Tired even after sleeping 😴
- Blurry vision 👓
Low Blood Sugar Clues (Hypoglycemia):
- Shaky or sweaty 💦
- Sudden hunger 🍎
- Confused or irritable 😠
- Fast heartbeat 💓
Teach them: “If you feel shaky or sweaty, eat 15g of fast sugar — like 4 oz juice or 3 glucose tabs. Wait 15 minutes. Check again.”
Step 5: Simplify the Treatment Plan — Focus on “What You DO”
Patients remember actions better than concepts.
“Managing diabetes isn’t about perfection. It’s about patterns. Small steps every day add up.”
Break it into 3 pillars:
- Food: “Eat balanced meals — carbs + protein + healthy fats. No need to ‘quit sugar’ — just control portions. A fist-sized carb portion per meal is a good start.”
- Movement: “Walk 10 minutes after meals. That’s it. It lowers blood sugar better than waiting.”
- Medication/Monitoring: “Take meds as scheduled. Check sugar like checking your phone — make it routine. Use alarms if needed.”
📌 Real-Life Case: Maria, 58, lowered her A1C from 9.2% to 6.8% in 4 months by walking after dinner and using a phone reminder for her metformin. No drastic diet. No gym. Just consistency.
Step 6: Address Fears & Myths — Gently and Directly
Common patient fears:
- “Will I need shots forever?” → “Maybe. But today’s pens are tiny and almost painless. Many people say it’s easier than they thought.”
- “Is this my fault?” → “No. Type 2 has lifestyle links, but genes, age, and even stress play big roles. This isn’t punishment — it’s a manageable condition.”
- “Will I go blind or lose a foot?” → “Only if sugar stays high for years without control. With good habits, most people avoid serious problems.”
“The goal isn’t fear — it’s empowerment.”
— Certified Diabetes Care and Education Specialist (CDCES)
Step 7: Use Visuals or Handouts — Even Simple Ones Help
You don’t need fancy brochures. A hand-drawn plate on a napkin works:
1
[½ Plate Veggies] [¼ Plate Lean Protein] [¼ Plate Carbs]
Or show this:
“Fill half your plate with non-starchy veggies (spinach, broccoli, peppers). One quarter with protein (chicken, tofu, fish). One quarter with carbs (rice, pasta, potato). Simple. Balanced. Effective.”
Step 8: End With Hope — Not Doom
Say:
“Diabetes is a marathon, not a sprint. You don’t have to be perfect. Just consistent. Millions live full, active lives with diabetes — traveling, working, playing with grandkids. You’ve got this. And we’re here with you.”
Share success stories. Show before/after A1C charts. Celebrate small wins.
What NOT to Say When Explaining Diabetes
🚫 “You brought this on yourself.”
🚫 “Just lose weight and you’ll be fine.”
🚫 “If you don’t control this, you’ll lose your feet.”
🚫 “It’s not that serious.”
✅ Instead, try:
✔️ “This is new for you — and that’s okay.”
✔️ “We’ll figure this out together.”
✔️ “Small changes make a big difference.”
✔️ “You’re not alone — we’ve helped hundreds just like you.”
Tools & Resources to Share With Patients
- Free Apps: MySugr, Glucose Buddy (track sugar, meals, meds)
- YouTube Channels: Diabetes Daily, Dr. B (short, clear videos)
- Printable Guides: ADA’s “My Plate” or “Carb Counting Made Easy”
- Support Groups: Local hospital programs or online (Beyond Type 1, Diabetes Sisters)
🔗 For deeper medical context, refer patients to the Wikipedia page on Diabetes Mellitus — it’s surprisingly well-sourced and updated.
FAQ Section: Common Questions About Explaining Diabetes to Patients
Q1: What’s the easiest way to explain insulin to someone with no science background?
A: “Insulin is like a key. Your body makes it to unlock your cells so sugar from food can enter and give you energy. In diabetes, either you don’t make the key (Type 1), or the lock is sticky and the key doesn’t work well (Type 2).”
Q2: How do I explain A1C without confusing them?
A: “A1C is like a report card for your blood sugar over 3 months. Normal is under 5.7%. Diabetes starts at 6.5%. Think of it as your ‘sugar average’ — we want to keep it as close to normal as safely possible.”
Q3: Should I mention complications right away?
A: Not in the first conversation. Focus first on understanding, daily management, and building confidence. Introduce complications later — framed as “what we’re preventing together” — once they’re engaged in care.
Q4: How do I handle a patient who’s in denial?
A: Meet them where they are. Say, “It’s okay to feel overwhelmed. Let’s just focus on one small step this week — like checking your sugar once a day or walking after dinner. We’ll build from there.”
Q5: What if the patient doesn’t speak English well?
A: Use pictures, gestures, and translation apps. The ADA offers free materials in Spanish, Chinese, Vietnamese, and more. Never assume understanding — ask them to repeat back in their own words.
Q6: How often should I revisit the explanation?
A: At every visit — but adjust depth. First visit: big picture. Second: deeper dive into meds or diet. Third: troubleshooting. Repetition builds retention. Use teach-back: “Can you explain this back to me like you’re telling a friend?”
Conclusion: Clarity + Compassion = Better Outcomes
Explaining diabetes to a patient isn’t about dumping facts — it’s about building understanding, reducing fear, and sparking action. When you use simple analogies, relatable examples, and a tone of partnership, patients don’t just hear you — they trust you. And that trust? That’s what turns diagnosis into control. That’s what prevents complications. That’s what saves lives.
✅ You’ve got the tools.
✅ You’ve got the words.
✅ You’ve got the heart.
Now go explain diabetes — not as a disease, but as a manageable condition. One conversation at a time.
Loved this guide? Share it with a colleague, nurse, or friend who talks to patients!
👉 Tweet this: “Explaining #diabetes doesn’t have to be hard. Here’s how to do it right → [Link] #DiabetesEducation #PatientCare”
Leave a Reply