Finding out you have gestational diabetes can feel overwhelming—but you’re not alone. Nearly 1 in 10 pregnant women in the U.S. develop this condition, according to the CDC. The good news? With the right gestational diabetes patient education, you can protect both your health and your baby’s. This guide gives you clear, actionable steps backed by medical experts—so you can navigate your pregnancy with confidence.
What Is Gestational Diabetes—and Why Does It Matter?
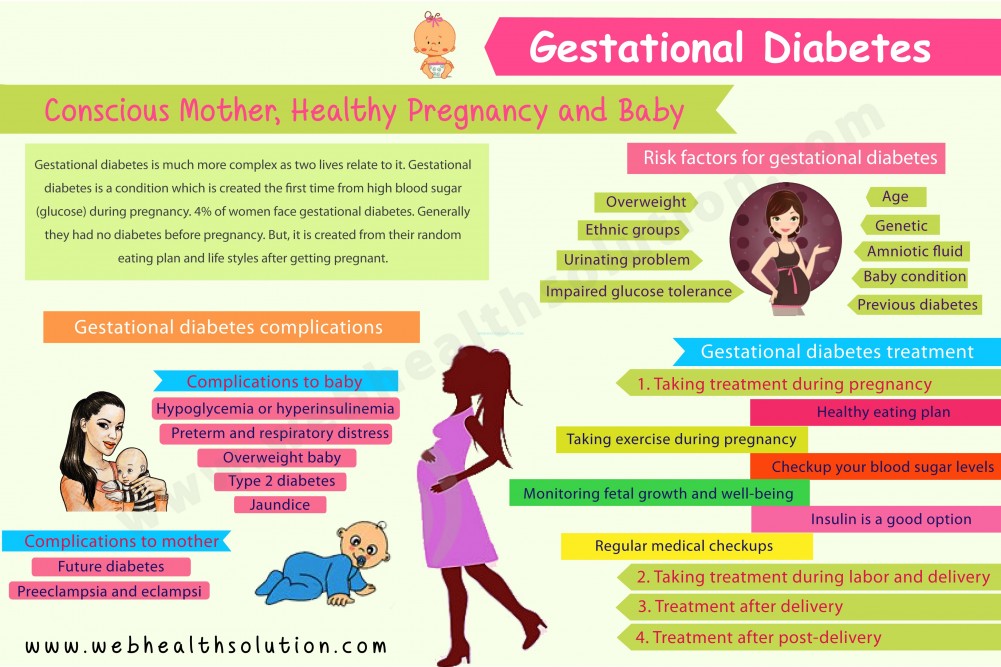
Gestational diabetes (GDM) is a type of high blood sugar that develops only during pregnancy, usually around the 24th to 28th week. Unlike type 1 or type 2 diabetes, it typically goes away after delivery—but if left unmanaged, it can lead to serious complications like:
- High birth weight (macrosomia)
- Preterm birth
- Increased risk of C-section
- Future risk of type 2 diabetes for both mother and child
According to the American College of Obstetricians and Gynecologists (ACOG), early detection and consistent management reduce these risks significantly. That’s where gestational diabetes patient education becomes your most powerful tool.
How Is Gestational Diabetes Diagnosed?
Most women are screened between 24 and 28 weeks of pregnancy using a two-step process:
- Glucose Challenge Test (GCT):
- Drink a sweet liquid containing 50 grams of glucose.
- Blood is drawn after 1 hour.
- If blood sugar is ≥140 mg/dL (or ≥130 mg/dL in some clinics), you’ll need a follow-up test.
- Oral Glucose Tolerance Test (OGTT):
- Fast overnight.
- Drink 100 grams of glucose solution.
- Blood is tested at fasting, then at 1, 2, and 3 hours.
- Diagnosis is confirmed if two or more values are above the threshold (e.g., fasting ≥95 mg/dL).
💡 Tip: Stay hydrated and avoid sugary foods the night before your test for more accurate results.
Managing Gestational Diabetes: A Step-by-Step Plan
Effective management hinges on three pillars: monitoring, nutrition, and activity. Here’s your practical roadmap:
Step 1: Monitor Blood Sugar Daily
Your healthcare team will likely ask you to check your levels four times a day:
- Fasting (before breakfast)
- 1 hour after breakfast
- 1 hour after lunch
- 1 hour after dinner
Target ranges (per ACOG guidelines):
- Fasting: ≤95 mg/dL
- 1 hour post-meal: ≤140 mg/dL
- 2 hours post-meal: ≤120 mg/dL
Use a reliable glucose meter and log results in an app or notebook. Consistency helps your provider adjust your plan quickly.
Step 2: Follow a Balanced Meal Plan
Work with a registered dietitian to create a personalized eating plan. General principles include:
- Carbohydrate control: Aim for 35–45% of daily calories from complex carbs (whole grains, legumes, vegetables).
- Protein at every meal: Helps stabilize blood sugar (e.g., eggs, Greek yogurt, lean chicken).
- Fiber-rich foods: At least 25–30g/day from fruits, veggies, and whole grains.
- Avoid sugary drinks: Replace soda and juice with water, unsweetened tea, or sparkling water.
🥗 Sample Snack Idea:
1 small apple + 1 tbsp almond butter = steady energy, no sugar spike.
Step 3: Stay Active Safely
Exercise improves insulin sensitivity. Aim for 30 minutes of moderate activity most days, such as:
- Brisk walking
- Prenatal yoga
- Swimming
Always consult your OB-GYN before starting a new routine—especially if you have other pregnancy complications.
Step 4: Take Medication If Needed
About 15–30% of women require insulin or metformin when diet and exercise aren’t enough. Don’t view this as failure—it’s a smart, proactive step to keep you and your baby safe.
What to Eat (and Avoid) with Gestational Diabetes
| Non-starchy vegetables (spinach, broccoli, peppers) | Sugary cereals and pastries |
| Lean proteins (fish, tofu, eggs) | Fruit juices and soda |
| Whole grains (quinoa, oats, brown rice) | White bread and white rice |
| Healthy fats (avocado, nuts, olive oil) | Processed snacks (chips, cookies) |
Remember: Portion control matters. Even healthy carbs can raise blood sugar if eaten in large amounts.
For more on how insulin resistance works during pregnancy, see this overview on gestational diabetes from Wikipedia .
Real-Life Success: Maria’s Story
Maria, 32, was diagnosed with GDM at 26 weeks. “I panicked at first,” she says. “But my care team gave me clear gestational diabetes patient education—meal plans, glucose logs, even a walking group with other moms.”
She tracked her sugars daily, swapped white rice for quinoa, and walked 20 minutes after dinner. By 36 weeks, her levels were consistently in range—and she delivered a healthy 7 lb 2 oz baby girl. “Knowledge really was power,” she adds.
Common Myths About Gestational Diabetes—Busted
❌ Myth: “I caused this by eating too much sugar.”
✅ Truth: GDM is caused by pregnancy hormones that block insulin—not your diet alone. Risk factors include age, BMI, family history, and ethnicity.
❌ Myth: “I’ll definitely get type 2 diabetes later.”
✅ Truth: While risk increases (up to 50% over 10 years), lifestyle changes postpartum can reduce it dramatically.
❌ Myth: “My baby will be born with diabetes.”
✅ Truth: Babies aren’t born with diabetes, but they may have low blood sugar temporarily after birth—easily managed in the hospital.
FAQ: Gestational Diabetes Patient Education
Q: Can I prevent gestational diabetes?
A: Not always—but you can lower your risk. Maintain a healthy weight before pregnancy, stay active, and eat a balanced diet. If you’ve had GDM before, your risk rises to ~50% in future pregnancies, so early screening is key.
Q: Will I need to keep testing after delivery?
A: Yes. Most providers recommend a 2-hour glucose tolerance test 6–12 weeks postpartum to ensure blood sugar has returned to normal. Even if it has, get screened for type 2 diabetes every 1–3 years.
Q: Can I still have a vaginal birth?
A: Absolutely! Many women with well-controlled GDM deliver vaginally. Your care team will monitor baby’s size and your progress closely.
Q: Are artificial sweeteners safe during pregnancy?
A: Most FDA-approved sweeteners (like stevia, sucralose, aspartame) are considered safe in moderation. However, natural options like small portions of fruit are preferred.
Q: How does stress affect gestational diabetes?
A: High stress can raise cortisol, which increases blood sugar. Practice relaxation techniques—deep breathing, meditation, or prenatal massage—to help manage levels.
Q: What if I go past my due date?
A: Women with GDM are often induced by 39–40 weeks to reduce risks of stillbirth or complications from a large baby. Your OB will discuss the best timing for you.
Conclusion: You’ve Got This—with the Right Support
Gestational diabetes patient education isn’t just about numbers—it’s about empowerment. With smart choices, consistent monitoring, and a supportive care team, you can have a healthy pregnancy and a healthy baby.
👉 Share this guide with a friend or family member who’s expecting—it might be the resource they’ve been searching for!
Stay informed. Stay calm. And remember: you’re doing an amazing job.
Leave a Reply