If you’ve ever searched “explain diabetes to me,” you’re not alone. Millions of Americans are newly diagnosed—or know someone who is—and feel overwhelmed by confusing medical terms and conflicting advice. You deserve a clear, compassionate explanation that cuts through the noise. In this guide, we’ll break down diabetes in plain English, using trusted science and real-world insights so you can understand it, manage it, or support someone who does.
What Exactly Is Diabetes?
Diabetes isn’t just “high blood sugar”—it’s a chronic condition where your body struggles to use glucose (sugar) for energy. Glucose comes from the food you eat, and insulin—a hormone made by your pancreas—acts like a key to unlock your cells so glucose can enter.
When this system breaks down, glucose builds up in your blood, leading to serious health issues over time. According to the CDC, 38.4 million Americans—about 11.6% of the population—have diabetes, and 1 in 5 don’t even know they have it.
Understanding the type of diabetes you or a loved one has is the first step toward effective management.
What Are the Different Types of Diabetes?
Most people think there’s only one kind, but there are three main types, each with distinct causes and treatments:
1. Type 1 Diabetes
- Onset: Usually in childhood or young adulthood (but can occur at any age).
- Cause: An autoimmune reaction destroys insulin-producing cells in the pancreas.
- Treatment: Requires daily insulin injections or an insulin pump—for life.
- Prevalence: About 5–10% of all diabetes cases.
2. Type 2 Diabetes
- Onset: Typically in adults over 45, but rising in younger people due to obesity and sedentary lifestyles.
- Cause: Cells become resistant to insulin, and the pancreas can’t make enough to compensate.
- Treatment: Managed with diet, exercise, oral meds, and sometimes insulin.
- Prevalence: Roughly 90–95% of all diabetes cases in the U.S.
3. Gestational Diabetes
- Onset: During pregnancy.
- Cause: Hormonal changes cause insulin resistance.
- Risk: Increases chances of Type 2 diabetes later for both mother and child.
- Management: Usually resolves after birth but requires careful monitoring.
💡 Did You Know? While Type 1 can’t be prevented, up to 90% of Type 2 cases can be delayed or avoided through lifestyle changes (per the American Diabetes Association).
What Are the Common Signs and Symptoms?
Many symptoms sneak up slowly—especially with Type 2—so they’re often ignored. Watch for these red flags:
- Frequent urination (especially at night)
- Excessive thirst or hunger
- Unexplained weight loss
- Fatigue or blurred vision
- Slow-healing sores or frequent infections
- Tingling or numbness in hands or feet
Important: If you have any of these symptoms, see a doctor. Early diagnosis can prevent complications like heart disease, kidney failure, or vision loss.
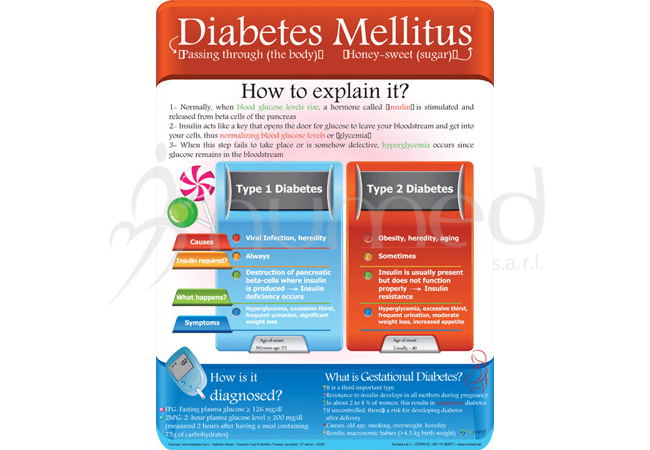
How Is Diabetes Diagnosed?
Doctors use simple blood tests to confirm diabetes:
| Fasting Plasma Glucose | < 100 mg/dL | ≥ 126 mg/dL |
| A1C (3-month average) | < 5.7% | ≥ 6.5% |
| Oral Glucose Tolerance | < 140 mg/dL | ≥ 200 mg/dL |
An A1C test is the most common—it shows your average blood sugar over 2–3 months without fasting. No guesswork, just clarity.
For more on diagnostic criteria, see the CDC’s diabetes page .
Can You Reverse or Cure Diabetes?
Let’s be honest: Type 1 diabetes cannot be cured—yet. But with modern tech (like continuous glucose monitors and smart insulin pumps), people live full, active lives.
Type 2 is different. While not “cured,” it can go into remission. A landmark 2017 UK study (DiRECT trial) found that 46% of participants reversed Type 2 diabetes after losing 10+ kg (22+ lbs) through a structured weight-loss program.
Key steps for remission:
- Lose 5–10% of your body weight (even 10–15 lbs helps).
- Eat whole foods: vegetables, lean protein, healthy fats—limit processed carbs.
- Move daily: Aim for 150 minutes of moderate exercise per week (e.g., brisk walking 30 mins, 5 days/week).
- Monitor blood sugar regularly.
🩺 Expert Insight: “Remission isn’t magic—it’s biology. Reduce fat in the liver and pancreas, and insulin function often improves,” says Dr. Roy Taylor, lead researcher of the DiRECT trial.
Daily Management: What Does Living With Diabetes Look Like?
Managing diabetes isn’t about perfection—it’s about consistency. Here’s a realistic daily routine:
Morning
- Check fasting blood sugar (target: 80–130 mg/dL).
- Take prescribed meds or insulin.
- Eat a balanced breakfast (e.g., eggs + avocado + whole-grain toast).
Meals
- Follow the “plate method”: ½ non-starchy veggies, ¼ lean protein, ¼ whole grains.
- Limit sugary drinks—opt for water, unsweetened tea, or sparkling water.
Evening
- Check blood sugar 1–2 hours after dinner (target: < 180 mg/dL).
- Take a 15-minute walk after meals to lower glucose spikes.
Weekly
- Log your numbers in an app (like MySugr or Glucose Buddy).
- Schedule a 30-minute call with a certified diabetes care specialist (many insurance plans cover this).
Type 1 vs Type 2 Diabetes: Key Differences at a Glance
| Cause | Autoimmune | Insulin resistance |
| Onset | Sudden (weeks) | Gradual (years) |
| Insulin Needed? | Always | Sometimes |
| Preventable? | No | Often yes |
| Avg. Age at Diagnosis | < 30 | > 45 |
| Body Weight | Often normal or underweight | Often overweight |
Understanding these differences helps avoid stigma—diabetes is not caused by “eating too much sugar.” Genetics, environment, and biology all play roles.
FAQ: Your Top Questions Answered
Q: Can kids get Type 2 diabetes?
A: Yes. Once rare in children, Type 2 now accounts for up to 1 in 3 new diabetes cases in teens (per CDC data). Rising obesity rates are a major factor. Early screening is critical for at-risk youth.
Q: Is prediabetes serious?
A: Absolutely. Prediabetes means your blood sugar is higher than normal but not yet diabetic. 96 million U.S. adults have it—and without action, 15–30% will develop Type 2 within 5 years. The good news? Lifestyle changes can reverse it.
Q: Do I need to avoid all carbs?
A: No! Carbs aren’t the enemy—quality and quantity matter. Choose complex carbs (oats, beans, sweet potatoes) over refined ones (white bread, soda). Work with a dietitian to find your ideal carb intake.
Q: Can stress affect blood sugar?
A: Yes. Stress hormones like cortisol raise glucose levels. Practice stress-reduction techniques: deep breathing, walking in nature, or 10 minutes of meditation daily.
Q: Are there new treatments on the horizon?
A: Exciting advances are underway! Artificial pancreas systems, once experimental, are now FDA-approved. Researchers are also testing stem cell therapies for Type 1 and GLP-1 drugs (like Ozempic) for weight and glucose control in Type 2.
Conclusion: Knowledge Is Power
Now that we’ve helped explain diabetes to you, you’re better equipped to take control—whether for yourself or someone you care about. Diabetes is serious, but it doesn’t have to define your life. With early action, smart habits, and support, millions live healthy, vibrant lives.
👉 Found this helpful? Share it with a friend or family member who’s searching “explain diabetes to me.” A single click could spark their journey to better health.
Remember: You’re not alone. Trusted resources like the American Diabetes Association and your healthcare team are here to help every step of the way.
Leave a Reply