Living with diabetes isn’t just about monitoring blood sugar—it’s a daily journey filled with physical, emotional, and logistical challenges. Patients with diabetes experience everything from fluctuating energy levels to complex medication routines, often while juggling work, family, and social life. If you or someone you love has been diagnosed, you’re not alone: over 37 million Americans live with diabetes today (CDC, 2023). Understanding what they truly go through is the first step toward better support, management, and quality of life.
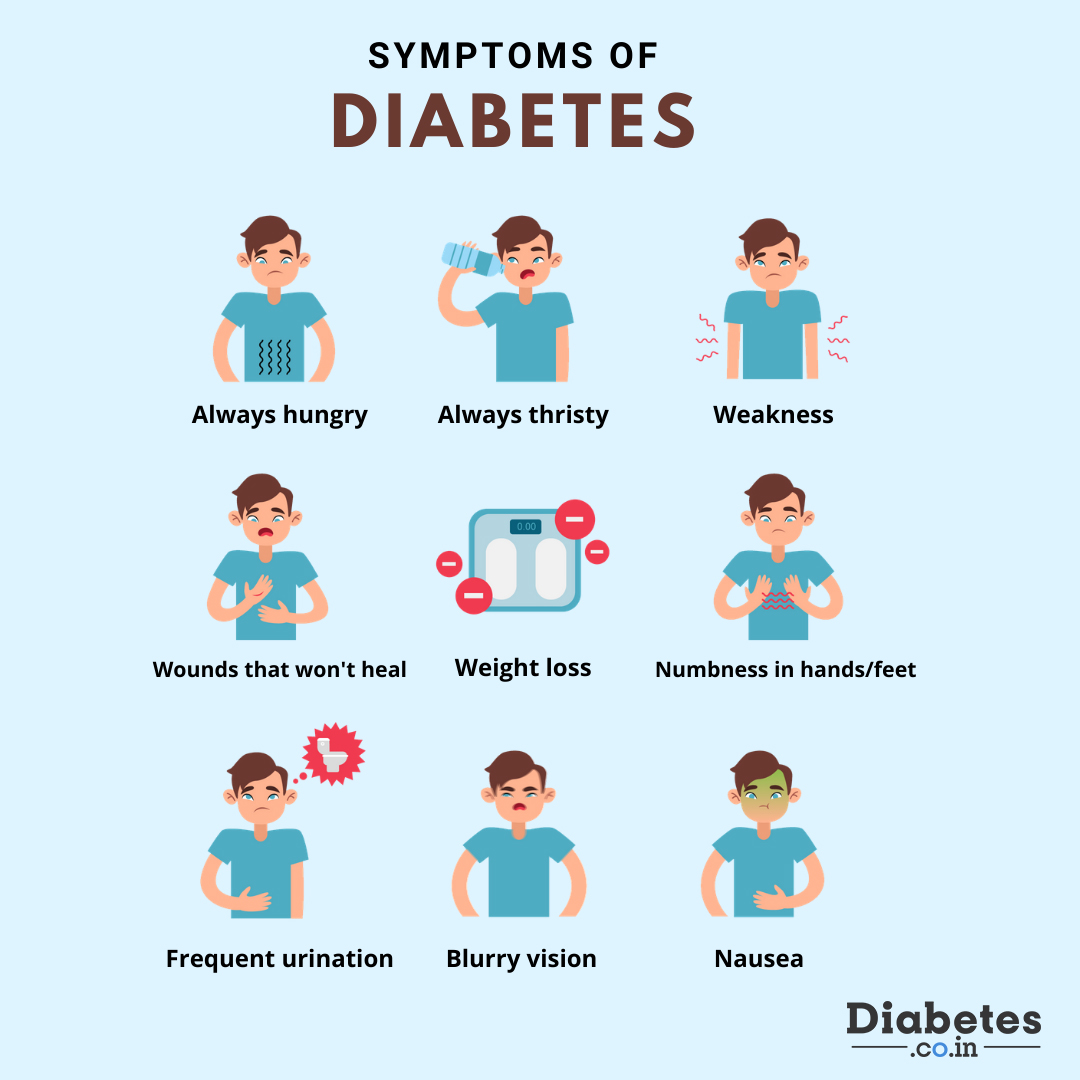
What Symptoms Do Patients With Diabetes Experience?
Early signs of diabetes can be subtle but disruptive. According to the American Diabetes Association (ADA), common symptoms include:
- Frequent urination (especially at night)
- Excessive thirst and hunger
- Unexplained weight loss (more common in Type 1)
- Fatigue and blurred vision
- Slow-healing sores or frequent infections
For Type 2 diabetes—which accounts for 90–95% of all cases—symptoms may develop gradually and go unnoticed for years. In contrast, Type 1 often appears suddenly, especially in children and young adults.
“Many patients tell me they dismissed their fatigue as ‘just stress’ until their blood sugar hit dangerous levels,” says Dr. Lisa Chen, endocrinologist at Johns Hopkins Medicine.
How Does Diabetes Affect Daily Life?
Managing diabetes isn’t a once-a-day task—it’s woven into nearly every moment. Here’s what a typical day might look like:
Morning Routine
- Check fasting blood glucose (target range: 80–130 mg/dL)
- Administer insulin (for Type 1 or advanced Type 2)
- Plan breakfast with carb counting (e.g., 30g carbs = 1 slice toast + 1 egg + ½ banana)
Work & Social Challenges
- Need to carry snacks to prevent hypoglycemia
- Explain dietary restrictions at meetings or dinners
- Manage stress, which can spike blood sugar
Nighttime Concerns
- Risk of nocturnal hypoglycemia (low blood sugar during sleep)
- Continuous Glucose Monitors (CGMs) may beep, disrupting rest
A 2022 study in Diabetes Care found that 68% of adults with diabetes report diabetes-related distress—a mix of burnout, anxiety, and frustration—that impacts adherence to treatment.

Emotional & Psychological Impact
Patients with diabetes experience more than physical symptoms—they often face invisible emotional burdens:
- Diabetes distress: Feeling overwhelmed by self-care demands
- Anxiety about complications (e.g., neuropathy, vision loss)
- Social stigma: Misconceptions like “You caused this by eating sugar”
The ADA emphasizes that mental health is part of diabetes care. Therapy, support groups, and mindfulness practices can significantly improve outcomes.
Tip: The CDC’s National Diabetes Prevention Program includes stress management modules proven to reduce HbA1c levels by 0.5–1.0% over 12 months.
Managing Diabetes: Practical Strategies That Work
You don’t need perfection—just consistent, informed choices. Here’s a step-by-step approach:
Step 1: Monitor Blood Sugar Regularly
- Use a glucometer (finger-prick) or CGM (continuous monitor)
- Track patterns: high after meals? Low during exercise?
Step 2: Build a Balanced Plate
Follow the “Plate Method” (recommended by ADA):
- ½ plate non-starchy veggies (spinach, broccoli, peppers)
- ¼ plate lean protein (chicken, tofu, fish)
- ¼ plate whole grains or starchy veg (brown rice, sweet potato)
Step 3: Move Daily
- Aim for 150 minutes/week of moderate activity (e.g., brisk walking)
- Even 10-minute walks after meals lower post-meal glucose spikes
Step 4: Medication Adherence
- Set phone reminders for insulin or oral meds
- Never skip doses—even if you “feel fine”
For more on diabetes types and mechanisms, see the Wikipedia overview on diabetes mellitus , a reliable starting point for understanding pathophysiology.
Technology & Tools: Game Changers for Modern Management
| CGMs | Real-time glucose trends, alerts for highs/lows | Cost (~$300/month without insurance) |
| Insulin Pumps | Precise dosing, fewer injections | Learning curve; not for all patients |
| Diabetes Apps(e.g., MySugr, Glucose Buddy) | Log food, meds, activity in one place | Data privacy varies by app |
Many patients report 30–50% fewer ER visits after adopting CGMs, per a 2021 JAMA study.
Support Systems: You Don’t Have to Do It Alone
Strong support improves outcomes dramatically:
- Family involvement: Partners can learn to recognize hypoglycemia signs (shaking, confusion, sweating)
- Online communities: Platforms like Beyond Type 1 or TuDiabetes offer peer advice
- Healthcare team: Endocrinologist, dietitian, diabetes educator—schedule visits every 3–6 months
“The most successful patients I see treat diabetes as a team sport,” says certified diabetes care specialist Maria Lopez, RD.
FAQ: Common Questions About Living With Diabetes
Q: Can patients with diabetes eat sugar?
A: Yes—in moderation and as part of a balanced meal plan. The key is portion control and timing. A small dessert after a high-fiber meal causes less glucose spike than eating it on an empty stomach.
Q: Do all patients with diabetes need insulin?
A: No. All Type 1 patients require insulin, but many with Type 2 manage with oral meds, diet, and exercise—especially early on. Over time, some may need insulin as the disease progresses.
Q: How often should blood sugar be checked?
A: It varies. Those on insulin may test 4–10 times/day. Others might check once daily or a few times per week. Follow your doctor’s recommendation based on your treatment plan.
Q: Can stress really affect blood sugar?
A: Absolutely. Stress hormones like cortisol raise blood glucose. Techniques like deep breathing (5 minutes, 2x/day) or yoga can help stabilize levels.
Q: Is diabetes reversible?
A: Type 1 is not reversible. However, Type 2 can go into remission—especially with significant weight loss (5–10% of body weight) and sustained lifestyle changes. Remission means normal blood sugar without meds, but monitoring remains essential.
Q: What’s the biggest mistake newly diagnosed patients make?
A: Trying to do everything perfectly overnight. Start with one change—like walking 15 minutes after dinner—then build from there. Progress > perfection.
Conclusion
Patients with diabetes experience a complex mix of physical, emotional, and practical challenges—but with the right tools, support, and mindset, they can live full, healthy lives. From smart tech to mindful eating and strong community ties, every small step adds up to better control and peace of mind.
If this article helped you understand what life with diabetes really looks like, share it with someone who might benefit—on Facebook, Twitter, or via email. Knowledge is power, and support starts with awareness.
Remember: You’re not managing a number—you’re nurturing a life. 💙
Leave a Reply