You’re Not Alone — And Recovery Is Possible
If you’ve been diagnosed with diabetes — especially Type 2 — you’re probably wondering: “How long until I feel better? Can I ever get off meds? What’s my real Diabetes Recovery Time?”
You’re not broken. You’re not doomed. And yes — with the right steps, many people significantly reverse insulin resistance, normalize blood sugar, and reclaim their energy. Let’s walk through what “recovery” really means, how long it typically takes, and exactly what you can do to speed it up — safely and sustainably.
What Does “Diabetes Recovery Time” Actually Mean?
Before we dive into timelines, let’s clarify: “Recovery” doesn’t always mean “cure.” In medical terms, we often refer to remission — when your blood sugar levels stay in the normal range without medication for at least 3 months.
According to the American Diabetes Association (ADA), remission is categorized as:
- Partial remission: HbA1c <6.5% for at least 1 year without meds
- Complete remission: HbA1c <5.7% (non-diabetic range) for 1 year
- Prolonged remission: Complete remission lasting 5+ years
“Remission is achievable — especially in the first 10 years after diagnosis. The pancreas often retains the ability to recover if we reduce fat in the liver and pancreas.” — Prof. Roy Taylor, Newcastle University, UK
How Long Is Typical Diabetes Recovery Time?
There’s no universal clock. But based on clinical studies and real-world data, here’s what most people experience:
⏱️ Short-Term Improvements (2–8 Weeks)
- Fasting blood sugar drops by 20–50 mg/dL
- Energy levels improve
- Reduced brain fog and cravings
- Example: A 2021 study in Diabetes Care showed participants lowered HbA1c by 1.3% in just 8 weeks with a low-calorie diet.
📅 Mid-Term Remission (3–6 Months)
- Many achieve partial or complete remission
- Medication reduction or elimination (under doctor supervision)
- Weight loss of 10–15% body weight often triggers metabolic reset
🎯 Long-Term Maintenance (1+ Years)
- Sustained normal blood sugar
- Lifestyle becomes habit, not effort
- Risk of complications (neuropathy, retinopathy) significantly reduced
💡 Key Insight: The Diabetes Remission Clinical Trial (DiRECT) found that 46% of participants achieved remission at 1 year — and 36% remained in remission at 2 years — through structured weight management.
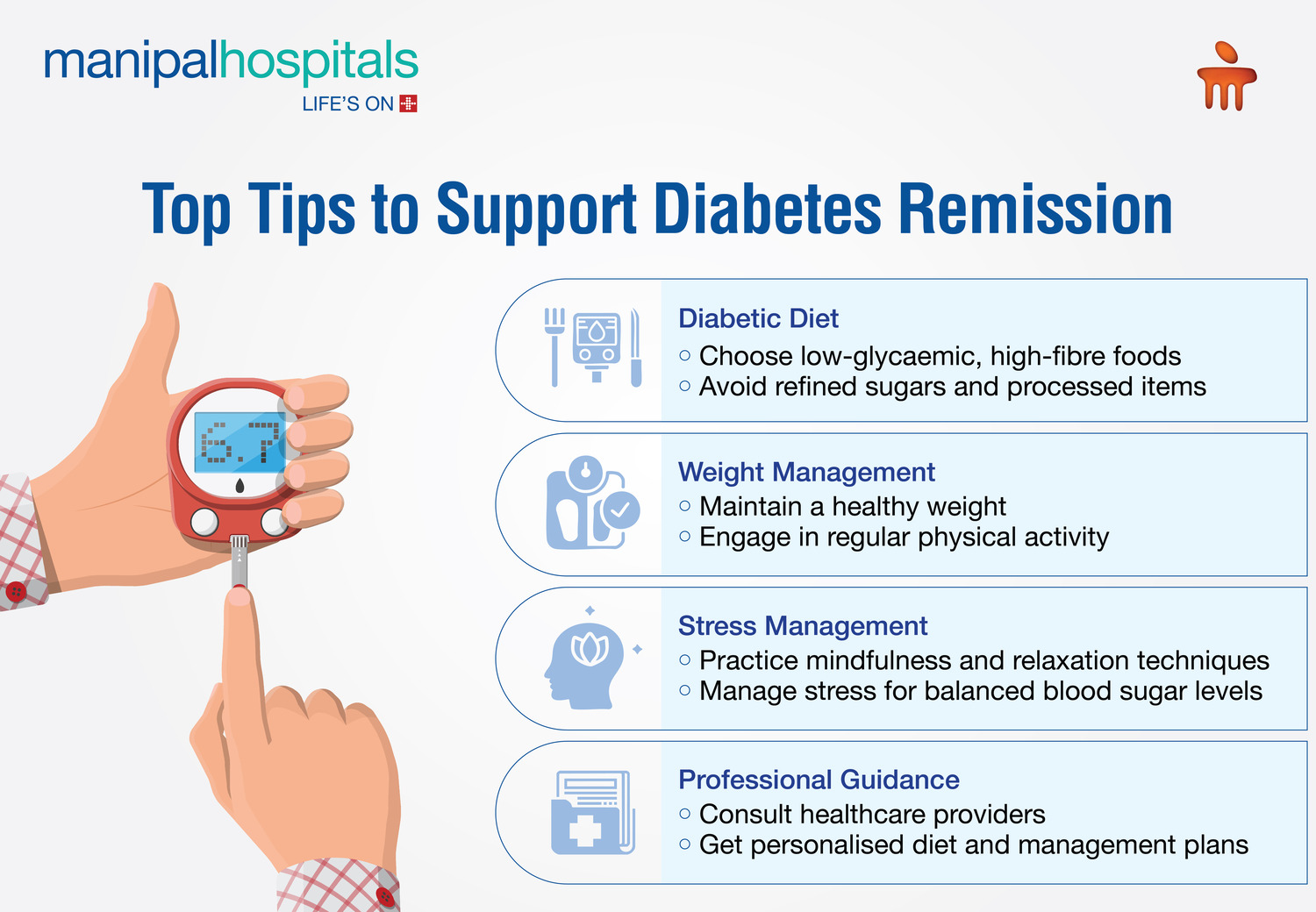
5 Proven Steps to Shorten Your Diabetes Recovery Time
You don’t need magic. You need method. Here’s your step-by-step roadmap:
Step 1: Reduce Liver & Pancreatic Fat (Weeks 1–4)
- Goal: Lose 5–10% of body weight rapidly (safely)
- How:
- Eat 800–1,200 calories/day for 8–12 weeks (meal replacements or whole foods)
- Focus on low-glycemic veggies, lean protein, healthy fats
- Avoid sugar, refined carbs, fried foods
- Science: Fat clogs insulin-producing cells. Removing it restores function. (Source: Wikipedia – Diabetes Mellitus )
Step 2: Move Daily — Even Just 20 Minutes (Start Day 1)
- Ideal: 150 mins/week moderate activity (brisk walking, cycling, swimming)
- Bonus: Add 2x/week resistance training (builds muscle = better glucose uptake)
- Pro Tip: Walk 10 mins after each meal — drops post-meal glucose by 20–30%
Step 3: Prioritize Sleep & Stress Management (Ongoing)
- Poor sleep → ↑ cortisol → ↑ blood sugar
- Aim for 7–8 hours/night
- Try 10-min daily meditation or deep breathing — proven to lower HbA1c
Step 4: Track & Tweak (Weekly Check-Ins)
- Test fasting glucose 3x/week (target: 70–99 mg/dL)
- Check HbA1c every 3 months
- Adjust calories/carbs if progress stalls
Step 5: Build Sustainable Habits (Months 3–6+)
- Transition from “diet” to lifestyle
- Cook 5+ meals/week at home
- Find enjoyable movement (dancing, gardening, pickleball)
- Join support groups — accountability boosts success by 3x
Type 1 vs Type 2 Diabetes: Recovery Time Differences
| Cause | Autoimmune — pancreas stops making insulin | Insulin resistance + relative deficiency |
| Recovery Possible? | No — lifelong insulin needed | Yes — remission common with lifestyle |
| Typical Timeline | N/A | 3–12 months for significant improvement |
| Key Strategy | Insulin dosing + tech (CGM/pump) | Weight loss + carb control + activity |
❗ Important: Type 1 cannot be reversed. But blood sugar control can improve dramatically with tech and precision dosing — reducing complications and improving quality of life.

Real Success Story: Maria’s 6-Month Turnaround
Maria, 52, diagnosed with Type 2 diabetes (HbA1c 8.9%). She followed this plan:
- Month 1–3: 900-calorie meal replacement plan + daily walks
- Month 4–6: Transitioned to whole-food low-carb diet + strength training 2x/week
- Result:
- Lost 38 lbs
- HbA1c dropped to 5.6%
- Off metformin and glipizide
- Energy restored, no more foot numbness
“I thought I’d be on meds forever. Now I feel 10 years younger.” — Maria R., Ohio
What Slows Down Diabetes Recovery Time?
Avoid these common roadblocks:
- ❌ Inconsistent eating — skipping meals or bingeing
- ❌ Sedentary lifestyle — sitting >8 hours/day
- ❌ Poor sleep hygiene — screens before bed, irregular hours
- ❌ Stress overload — cortisol spikes blood sugar
- ❌ Unrealistic expectations — expecting overnight miracles
🚫 Myth: “I need to lose 50 lbs to see results.”
✅ Truth: Losing just 5–7% of body weight can trigger remission for many.
Diabetes Recovery Time: FAQ Section
Q1: Can diabetes be reversed permanently?
A: “Reversed” is misleading. “Remission” is accurate. Many stay in remission 5+ years — but slipping back into old habits can bring diabetes back. Maintenance is lifelong.
Q2: How fast can HbA1c drop with lifestyle changes?
A: Many see 1.0–2.0% drop in 3 months. In DiRECT trial, average drop was 1.4% at 12 months. Faster drops occur with aggressive (but supervised) calorie restriction.
Q3: Do I still need to test blood sugar if I’m in remission?
A: Yes — at least quarterly. Remission isn’t cure. Annual HbA1c and occasional fasting glucose checks are wise to catch relapse early.
Q4: Can supplements speed up recovery?
A: No magic pills. Some like berberine or magnesium may help — but diet, exercise, and weight loss are 90% of the solution. Always consult your doctor.
Q5: Is bariatric surgery faster than diet for recovery?
A: Often yes — 60–80% achieve remission within weeks/months post-surgery. But it’s invasive and not for everyone. Lifestyle changes remain first-line per ADA guidelines.
Q6: What if I have complications — can I still recover?
A: Yes — but focus shifts to halting progression and improving quality of life. Nerve pain, vision issues, or kidney function may improve with tight glucose control.
Final Thoughts: Your Journey Starts Today — Not “Someday”
Your Diabetes Recovery Time isn’t written in stone. It’s shaped by your choices — starting now. Whether you see changes in 3 weeks or 6 months, every healthy meal, every walk, every good night’s sleep… it all adds up.
You don’t need perfection. You need persistence.
🌟 Takeaway: Recovery isn’t about being “cured.” It’s about being empowered. You hold more control than you think.
Loved this guide? Share it with someone who needs hope — and a practical plan.
👉 Tag a friend. Save this. Print it. Start today.
Because your health isn’t a countdown.
It’s a comeback.
Leave a Reply