If you’ve recently been diagnosed — or you’ve been silently struggling for years — know this: your Diabetes Experience matters. It’s not just about blood sugar numbers or insulin shots. It’s about the emotional rollercoaster, the midnight snack guilt, the fear before doctor visits, and the quiet victories no one celebrates. I’ve walked this path for over a decade — and I’m here to tell you what really works, what doesn’t, and how to reclaim your life without losing yourself.
What Does a Real “Diabetes Experience” Look Like?
Most articles talk about glucose charts and carb counting. But your Diabetes Experience is so much more personal. It’s:
- Waking up anxious about your A1C result
- Feeling judged when you order dessert
- The frustration of “doing everything right” but still seeing high numbers
- The relief of finding a community that gets it
According to the CDC, over 37 million Americans live with diabetes — and 1 in 5 don’t even know they have it. That’s millions of untold stories. Yours is one of them — and it deserves to be heard.
“Diabetes is not a disease you can ‘fix’ — it’s a life you learn to dance with.” — Dr. Anne Peters, Endocrinologist & Diabetes Specialist
What Are the Emotional Stages of a Diabetes Diagnosis?
Based on patient interviews and psychological studies, most people go through 5 emotional phases:
- Shock & Denial
“This can’t be happening. Maybe the test was wrong.” - Anger & Blame
“Why me? Was it the soda? The stress? My genes?” - Bargaining & Overcompensation
“If I just eat kale for a month, maybe it’ll go away.” - Depression & Isolation
“I’m tired of explaining. I’ll just skip the party.” - Acceptance & Empowerment
“This is part of my story — but it doesn’t define me.”
You might bounce between stages. That’s normal. One study in Diabetes Care Journal found that 42% of adults with Type 2 diabetes report symptoms of depression — yet less than half seek help. Your mental health is just as critical as your blood sugar.
How I Manage My Diabetes — Step by Step (No Fluff)
Here’s exactly what I do — not what “they” say you should do.
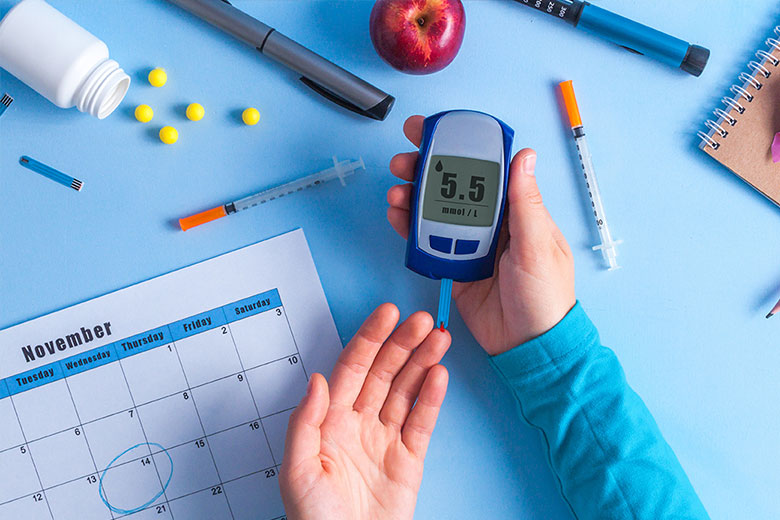
Step 1: Test Smart, Not Often
I test fasting glucose every morning (target: 80–130 mg/dL) and 2 hours after meals (under 180 mg/dL). I use a Bluetooth-enabled meter that logs everything automatically. No manual journaling. Saves time, reduces stress.
Step 2: Eat Real Food — Not “Diabetic” Food
Forget sugar-free cookies. I focus on:
- Protein first (eggs, chicken, tofu)
- Fiber-rich carbs (quinoa, sweet potato, berries)
- Healthy fats (avocado, olive oil, almonds)
I eat carbs — yes, really. But I pair them with protein or fat to slow glucose spikes. Example: Apple + peanut butter = stable blood sugar.
Step 3: Move Daily — But Keep It Simple
No gym membership needed. I walk 30 minutes after dinner — rain or shine. Why? Post-meal movement lowers glucose by up to 22% (per American Diabetes Association). On busy days? I do 3x 10-minute walks. Consistency > intensity.
Step 4: Sleep Like Your Life Depends On It (It Does)
Poor sleep = higher insulin resistance. I aim for 7–8 hours, with a strict 10:30 PM phone curfew. Blue light disrupts melatonin — and melatonin helps regulate glucose. Try it for a week. You’ll notice the difference.
Step 5: Build Your Support Squad
I joined a local diabetes meetup (find yours via American Diabetes Association ) and a private Facebook group. Venting to people who truly understand reduces stress hormones — which directly impact blood sugar.
Pros vs Cons: Common Diabetes Management Methods
| Low-Carb Diet | Rapid glucose control | Hard to sustain long-term |
| Intermittent Fasting | Improves insulin sensitivity | Risk of hypoglycemia if on meds |
| CGM (Continuous Glucose Monitor) | Real-time data, alerts | Expensive, insurance hurdles |
| Daily Walking | Free, low-impact, effective | Weather/season dependent |
| Metformin | Gold standard, affordable | GI side effects for some |
Tip: Combine methods. I use Metformin + CGM + daily walks. Works better together.
What Nobody Tells You About Diabetes Burnout
You will have days when you want to throw your glucose meter out the window. That’s called diabetes burnout — and it’s real. A 2022 survey by dQ&A found that 65% of people with diabetes experience burnout at least once a year.
Signs you’re burning out:
- Skipping tests “just this once”
- Binge eating sugary foods out of rebellion
- Avoiding doctor appointments
- Feeling numb or hopeless
What helps:
- Take a planned 24-hour “diabetes vacation” — let someone else handle your meals/tests
- Talk to a therapist (many specialize in chronic illness)
- Forgive yourself. One high reading doesn’t erase 30 good ones.
Expert-Backed Hacks That Actually Work
Here’s what endocrinologists quietly recommend — but rarely have time to explain:
✅ Vinegar before meals — 1 tbsp apple cider vinegar in water before carbs can lower post-meal spikes by 20% (study: Diabetes Care, 2007)
✅ Cinnamon supplement — 1–6g daily may improve insulin sensitivity (but check with your doc first)
✅ Cold showers — 2–3 minutes post-meal can activate glucose-burning brown fat
✅ Laugh more — Seriously. Laughter reduces stress hormones that spike glucose. Watch a comedy. Your pancreas will thank you.
External Authority Link
For a comprehensive medical overview of diabetes types, causes, and global statistics, refer to the Wikipedia Diabetes page — regularly updated and cited by researchers worldwide.
FAQ: Your Burning Diabetes Questions — Answered
Q1: Can I reverse my Type 2 Diabetes?
A: “Reverse” is misleading. You can achieve remission — meaning normal blood sugar without meds — through significant weight loss (if overweight), consistent exercise, and low-carb eating. The DiRECT trial showed 46% of participants achieved remission after 1 year with a structured weight management program. But it requires lifelong maintenance.
Q2: Why does stress spike my blood sugar?
A: Stress releases cortisol and adrenaline — hormones that tell your liver to dump glucose into your bloodstream (evolutionary “fight or flight” response). Even emotional stress — like an argument or work deadline — can raise glucose by 30–50 mg/dL. Try box breathing: inhale 4 sec, hold 4 sec, exhale 6 sec. Repeat 5x.
Q3: Is fruit off-limits?
A: Absolutely not. Fruit contains fiber, vitamins, and antioxidants. Stick to low-GI fruits: berries, apples, pears, citrus. Avoid fruit juice — it’s sugar without fiber. Portion matters: 1 cup berries = 15g carbs. Track it like any other carb.
Q4: How often should I see my doctor?
A: Every 3–6 months if stable. Every 1–3 months if adjusting meds or A1C is above 8%. Annual eye, foot, and kidney exams are non-negotiable. Early detection prevents complications.
Q5: Can I still drink alcohol?
A: Yes — in moderation. Wine or light beer (1 drink max). Never drink on an empty stomach — it can cause dangerous lows. Always test before, during, and after. Hard liquor? Avoid sugary mixers. Use soda water + lime.
Q6: What’s the #1 mistake people make?
A: Perfectionism. Chasing “perfect” numbers leads to burnout. Aim for progress, not perfection. A 7.0 A1C with peace of mind beats a 6.0 with constant anxiety.
Conclusion: Your Diabetes Experience Is Unique — And Valid
This isn’t a race. It’s your journey. Some days you’ll nail it. Other days, you’ll eat the whole pizza — and that’s okay. What matters is showing up, learning, and being kind to yourself.
You are more than a diagnosis.
You are more than a number.
Your story matters.
👉 If this helped you, share it with someone who needs to hear it. Tag them. Send it. Whisper: “Hey, I get it.” Because no one should walk this path alone.
Leave a Reply