If you or a loved one has diabetes, you might wonder: Can a diabetic patient experience hypoglycemia? The answer is yes—and it’s more common than many realize. Hypoglycemia (low blood sugar) is a serious, sometimes life-threatening condition that can affect anyone with diabetes, especially those using insulin or certain oral medications. Understanding how and why it happens is the first step toward staying safe and in control.
What Is Hypoglycemia—and Why Does It Happen in Diabetics?
Hypoglycemia occurs when blood glucose drops below 70 mg/dL. While it’s often associated with insulin-treated diabetes, it can also affect people with type 2 diabetes on specific medications like sulfonylureas or meglitinides.
According to the American Diabetes Association (ADA), nearly 4 in 10 people with type 1 diabetes experience at least one episode of severe hypoglycemia per year. Even among those with type 2 diabetes, up to 10–30% report frequent low blood sugar events—especially as treatment intensifies.
The core issue? An imbalance between insulin (or insulin-stimulating drugs), food intake, and physical activity. Too much medication, too little food, or unexpected exercise can tip the scale dangerously low.
💡 Key Insight: Hypoglycemia isn’t just “feeling shaky.” Left untreated, it can lead to confusion, seizures, unconsciousness, or even death.
For a deeper dive into the physiological mechanisms, see the Wikipedia entry on hypoglycemia .
Common Causes of Hypoglycemia in Diabetic Patients
Several factors can trigger low blood sugar in people with diabetes:
- Excess insulin or diabetes medication
- Skipping or delaying meals
- Unplanned or intense physical activity
- Alcohol consumption (especially without food)
- Incorrect carb-to-insulin ratio
- Kidney or liver dysfunction (which affects drug metabolism)
A 2022 study published in Diabetes Care found that evening alcohol intake increased nocturnal hypoglycemia risk by 3.5 times in insulin users—highlighting how lifestyle choices directly impact blood sugar stability.
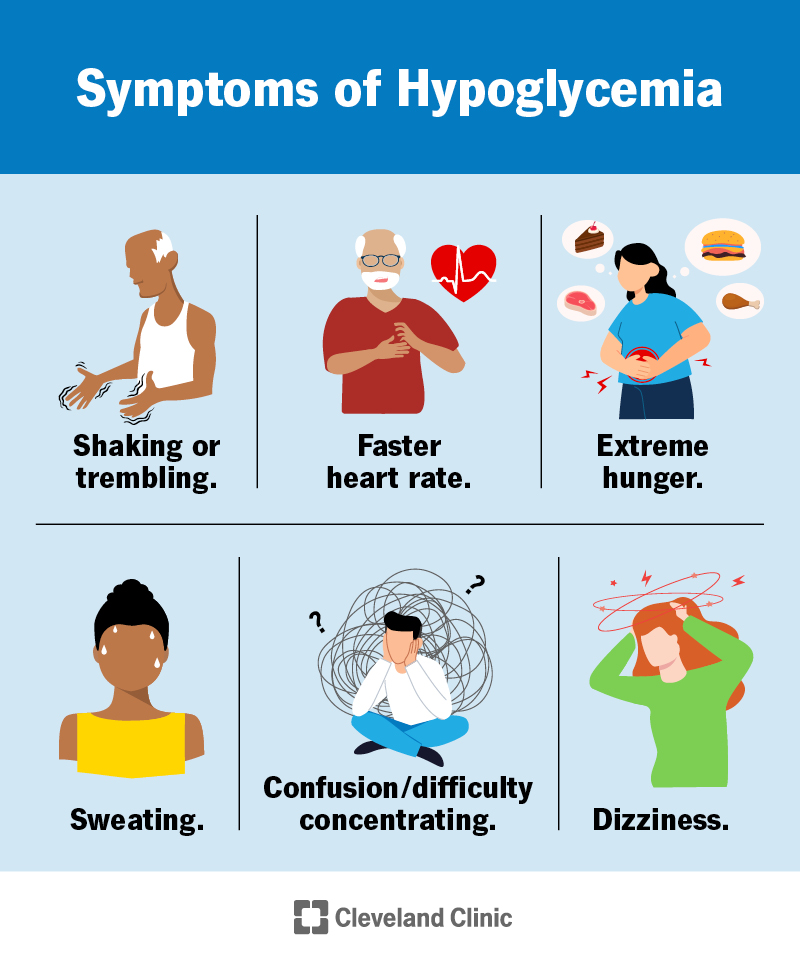
Recognizing the Signs: Hypoglycemia Symptoms to Watch For
Early detection saves lives. Symptoms typically appear when blood sugar falls below 70 mg/dL and progress in stages:
Mild to Moderate Symptoms:
- Shakiness or trembling
- Sweating (even when cool)
- Rapid heartbeat
- Hunger
- Dizziness or lightheadedness
- Irritability or anxiety
Severe Symptoms (Require Emergency Help):
- Confusion or disorientation
- Blurred vision
- Seizures
- Loss of consciousness
⚠️ Note: Some people—especially those with long-standing diabetes—develop hypoglycemia unawareness, where they no longer feel early warning signs. This condition increases the risk of severe episodes by up to 6-fold (ADA, 2023).
How to Treat Hypoglycemia: The 15-15 Rule (Step-by-Step)
If you suspect low blood sugar, act fast. Follow the 15-15 Rule, endorsed by the ADA:
- Check blood sugar (if possible). If it’s ≤70 mg/dL—or you can’t test but feel symptoms—proceed.
- Consume 15 grams of fast-acting carbs, such as:
- 4 oz (½ cup) of regular soda (not diet)
- 1 tablespoon of honey or sugar
- 3–4 glucose tablets
- ½ cup of fruit juice
- Wait 15 minutes, then recheck blood sugar.
- If still ≤70 mg/dL, repeat step 2.
- Once blood sugar is stable, eat a small snack or meal if your next meal is more than an hour away.
🚨 For severe hypoglycemia (unconsciousness or inability to swallow):
- Do NOT give food or drink (risk of choking).
- Administer glucagon (via injection or nasal spray) if available.
- Call 911 immediately.
Keep a glucagon kit accessible—and ensure family, coworkers, or roommates know how to use it.
Preventing Hypoglycemia: Practical Daily Strategies
Prevention is always better than emergency treatment. Here’s how to reduce your risk:
| Monitor blood sugar regularly | Catch trends before levels drop dangerously low |
| Eat consistent meals/snacks | Prevents large gaps in carb intake |
| Adjust insulin for activity | Reduce dose before exercise or add carbs |
| Limit alcohol | Always consume with food; avoid binge drinking |
| Use CGM (Continuous Glucose Monitor) | Alerts you to falling glucose in real time |
People using CGMs report 40% fewer hypoglycemic events compared to those relying solely on fingersticks (Journal of Clinical Endocrinology & Metabolism, 2021).
Also, talk to your doctor about medication review—some newer diabetes drugs (like SGLT2 inhibitors or GLP-1 agonists) carry lower hypoglycemia risk than older options.
Hypoglycemia vs. Hyperglycemia: Know the Difference
Many confuse low and high blood sugar. Here’s a quick comparison:
| Blood Sugar | <70 mg/dL | >180 mg/dL (often much higher) |
| Onset | Rapid (minutes) | Gradual (hours/days) |
| Key Symptoms | Sweating, shaking, hunger | Thirst, frequent urination, fatigue |
| Urgency | Immediate treatment needed | Monitor; may require insulin adjustment |
| Long-Term Risk | Accidents, coma | Nerve/kidney damage, heart disease |
Understanding this difference helps you respond correctly—and avoid dangerous mistakes (like giving insulin during hypoglycemia).
FAQ: Your Top Questions About Diabetic Hypoglycemia
Q1: Can someone with type 2 diabetes get hypoglycemia?
Yes. While more common in type 1, people with type 2 on insulin, sulfonylureas (e.g., glyburide), or meglitinides (e.g., repaglinide) are at significant risk.
Q2: Is hypoglycemia possible without diabetes?
Rarely—but yes. Conditions like insulinoma (a tumor), liver disease, or excessive alcohol can cause it. However, in the context of this article, we focus on diabetic hypoglycemia, which is far more prevalent.
Q3: How low is too low for blood sugar?
Below 70 mg/dL is clinically hypoglycemic. Levels under 54 mg/dL are considered clinically significant and require immediate action.
Q4: Can hypoglycemia happen at night?
Absolutely. Nocturnal hypoglycemia affects up to 50% of people with type 1 diabetes. Signs include nightmares, sweating through pajamas, or waking with a headache. Using a CGM with alarms can prevent this.
Q5: Should I carry glucose tablets?
Yes. Keep them in your car, purse, desk, and bedside. They’re fast, precise (15g per serving), and shelf-stable.
Q6: Can repeated hypoglycemia cause long-term brain damage?
In extreme, untreated cases—yes. But with proper management, the risk is minimal. More commonly, frequent lows lead to hypoglycemia unawareness, creating a dangerous cycle.
Conclusion: Stay Informed, Stay Safe
So, can a diabetic patient experience hypoglycemia? Absolutely—and understanding this risk empowers you to manage diabetes more safely and confidently. By recognizing early symptoms, treating lows promptly with the 15-15 rule, and adopting preventive habits (like consistent meals and glucose monitoring), you can significantly reduce your risk.
Your health is worth the extra attention. If this guide helped you, share it with someone who needs it—a friend, family member, or support group. Together, we can turn awareness into action.
📱 Found this helpful? Share on Facebook, Twitter, or WhatsApp to spread life-saving knowledge!
Leave a Reply