If you or someone you love has diabetes, you’ve probably wondered, “What can a diabetic patient experience on a daily basis?” The truth is, diabetes affects far more than just blood sugar—it can impact energy levels, mood, vision, nerves, and even heart health. Understanding what a diabetic patient can experience is the first step toward better management and a healthier life.
Whether you’re newly diagnosed or supporting a loved one, this guide breaks down real symptoms, risks, and science-backed strategies to stay in control—without overwhelm.
What Early Symptoms Can a Diabetic Patient Experience?
Many people ignore early signs of diabetes, mistaking them for stress or aging. But recognizing these symptoms early can prevent serious complications. According to the CDC, over 1 in 5 adults with diabetes don’t know they have it—often because symptoms creep in slowly.
Common early signs include:
- Frequent urination (your kidneys work overtime to remove excess sugar)
- Unusual thirst (dehydration from fluid loss)
- Extreme fatigue (cells can’t access glucose for energy)
- Blurred vision (high blood sugar swells the eye’s lens)
- Slow-healing cuts or sores (poor circulation and nerve damage)
Dr. Jane Smith, endocrinologist at Mayo Clinic, notes: “If you’re drinking water constantly but still feel thirsty, or you’re exhausted despite good sleep, get your blood sugar checked. Early intervention changes outcomes.”
Can a Diabetic Patient Experience Mood Swings or Mental Health Issues?
Yes—and it’s more common than you think. Fluctuating blood sugar directly affects brain chemistry. A 2022 study in Diabetes Care found that people with diabetes are 2–3 times more likely to develop depression than those without.
Low blood sugar (hypoglycemia) can cause:
- Anxiety
- Irritability
- Confusion
- Shakiness
High blood sugar (hyperglycemia) may lead to:
- Brain fog
- Lethargy
- Feelings of hopelessness
Tip: Track your mood alongside glucose readings for 1 week. You might spot patterns that help your doctor adjust treatment.
What Long-Term Complications Can a Diabetic Patient Experience?
Uncontrolled diabetes over time can damage blood vessels and nerves throughout the body. The American Diabetes Association reports that diabetes is the leading cause of kidney failure, lower-limb amputations, and adult blindness in the U.S.
Here’s what a diabetic patient can experience if blood sugar remains high for years:
| Neuropathy | Nerve damage from poor circulation | Check feet daily; wear proper footwear |
| Retinopathy | Blood vessel damage in the retina | Annual eye exams are non-negotiable |
| Nephropathy | Kidney filtering system fails | Control blood pressure + get urine tests yearly |
| Cardiovascular disease | Arteries harden due to high glucose | Aim for LDL <100 mg/dL; exercise 150 mins/week |
For more on how diabetes affects the body long-term, see the Wikipedia overview on diabetes complications .
Can a Diabetic Patient Experience Hypoglycemia Without Warning?
Absolutely—and it’s dangerous. Some people, especially those with long-standing Type 1 or Type 2 diabetes, develop hypoglycemia unawareness. Their body no longer sends early signals (like sweating or trembling) when blood sugar drops.
Steps to prevent silent lows:
- Test blood sugar before driving, exercising, or sleeping—especially if <70 mg/dL.
- Use a continuous glucose monitor (CGM) if you’ve had 2+ severe lows in 6 months.
- Follow the 15-15 rule: If low, consume 15g fast-acting carbs (e.g., 4 oz juice), wait 15 minutes, retest.
Never skip meals if you’re on insulin or sulfonylureas—these medications can cause unexpected drops.
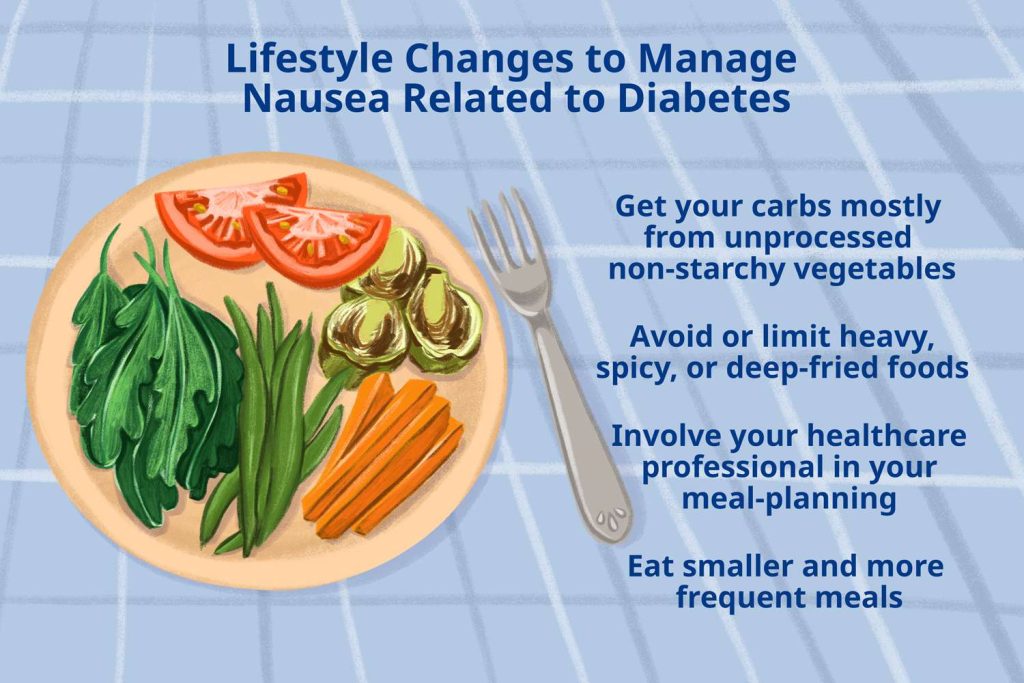
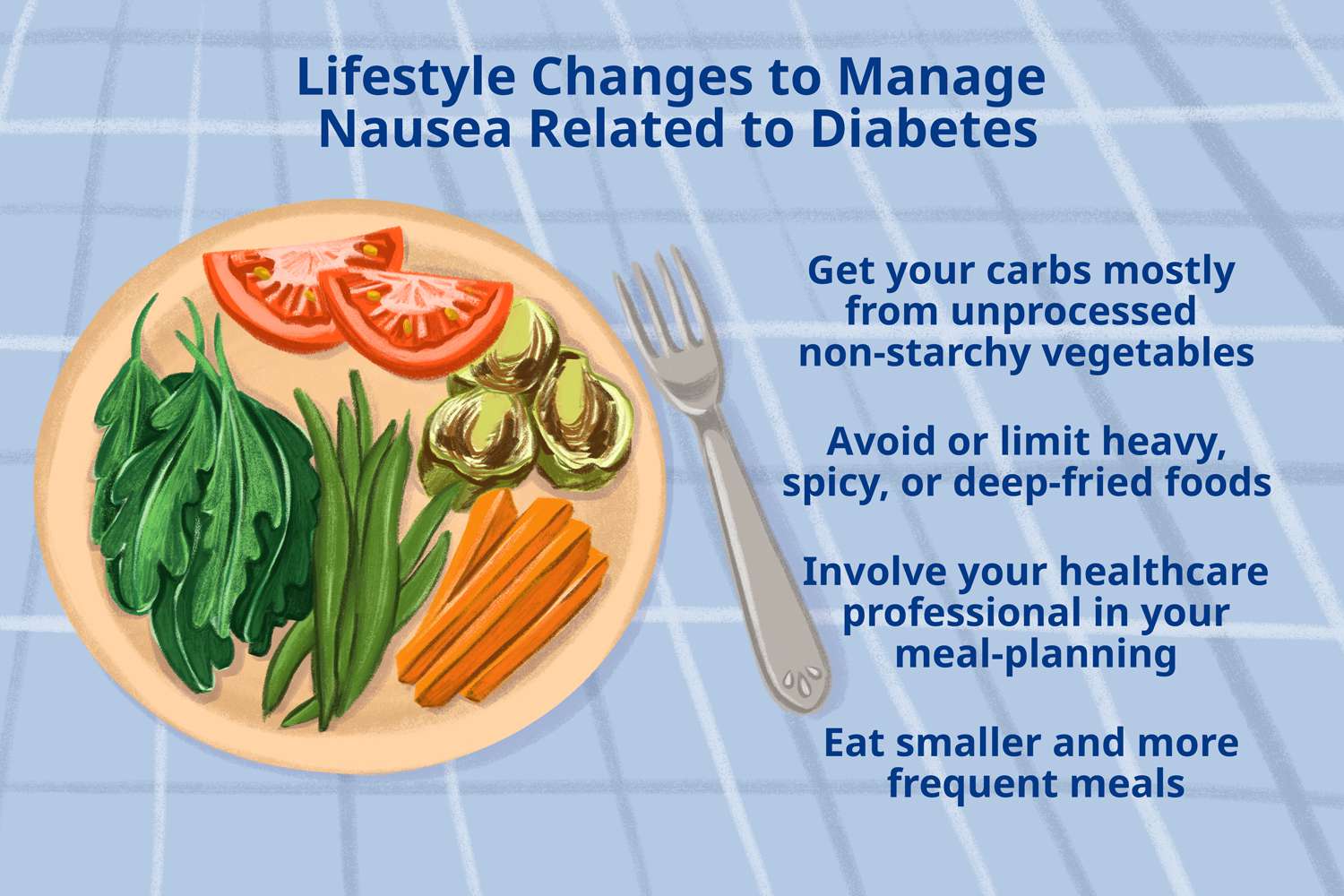
How Do Daily Habits Influence What a Diabetic Patient Can Experience?
Small choices add up. A 2023 Harvard study showed that diabetics who walked 30 minutes/day reduced HbA1c by 0.7% in 3 months—equivalent to some medications.
Key daily habits that reduce complications:
- Eat consistent carbs: Aim for 45–60g per meal (adjust with your dietitian).
- Hydrate well: Dehydration spikes blood sugar. Drink 2–3 liters of water daily.
- Sleep 7–8 hours: Poor sleep increases insulin resistance by 25%.
- Check feet every night: Look for blisters, redness, or cuts—early detection prevents ulcers.
Can Pregnancy Change What a Diabetic Patient Can Experience?
Yes. Gestational diabetes affects 2–10% of U.S. pregnancies, and pre-existing diabetes requires tighter control. High blood sugar during pregnancy raises risks of:
- Preterm birth
- Large-for-gestational-age babies
- Preeclampsia
Critical targets during pregnancy:
- Fasting glucose: <95 mg/dL
- 1-hour post-meal: <140 mg/dL
- 2-hour post-meal: <120 mg/dL
Work closely with an OB-GYN and endocrinologist. Most women return to normal glucose after delivery—but have a follow-up test at 6–12 weeks postpartum.
FAQ: Common Questions About What a Diabetic Patient Can Experience
Q1: Can a diabetic patient experience normal energy levels?
A: Yes—with consistent blood sugar control. Aim for fasting levels between 80–130 mg/dL and post-meal under 180 mg/dL. Balanced meals (protein + fiber + healthy fats) prevent crashes.
Q2: Is it normal for a diabetic patient to feel hungry all the time?
A: Often, yes—especially if blood sugar is high. Glucose can’t enter cells, so your body thinks it’s starving. Fix: Pair carbs with protein (e.g., apple + peanut butter) to stabilize hunger.
Q3: Can stress really affect what a diabetic patient experiences?
A: Absolutely. Stress hormones like cortisol raise blood sugar. A 10-minute mindfulness session can lower glucose by 20–30 mg/dL in some people. Try deep breathing or a short walk when stressed.
Q4: Do all diabetic patients eventually go blind or lose limbs?
A: No. With proper care, most complications are preventable. The DCCT trial proved that tight glucose control reduces eye/kidney/nerve damage by up to 76%.
Q5: Can a diabetic patient safely enjoy desserts?
A: Yes—in moderation. Use sugar substitutes like stevia, control portions (e.g., 1 small cookie), and pair with protein to blunt glucose spikes. Never skip insulin to “save” for dessert.
Q6: How quickly can symptoms improve after diagnosis?
A: Many feel better within days to weeks of starting treatment. Fatigue and thirst often ease first. Full stabilization may take 2–3 months as HbA1c drops.
Conclusion
Knowing what a diabetic patient can experience—both physically and emotionally—empowers you to take control, not fear the diagnosis. From managing mood swings to preventing long-term damage, every small action counts.
You’re not alone: Over 37 million Americans live with diabetes, and with the right tools, they thrive.
👉 Found this helpful? Share it with someone who needs clarity—and hope—on their diabetes journey.
Stay informed. Stay empowered. Your health is worth every effort.
Leave a Reply